-
PDF
- Split View
-
Views
-
Cite
Cite
Tae Nagama, Natsuko Kakudo, Atsuyuki Kuro, Yujiro Ozaki, Yasuko Shirasawa, Sakurako Kunieda, Kenji Suzuki, Fukuki Saito, Kenji Kusumoto, Full circumference lower extremity degloving injury treated with hydrosurgical debridement and negative-pressure wound therapy with gauze wound filler for fixation of avulsed flap skin grafts, Journal of Surgical Case Reports, Volume 2020, Issue 12, December 2020, rjaa498, https://doi.org/10.1093/jscr/rjaa498
Close - Share Icon Share
Abstract
Degloving, a skin and subcutis avulsion, is a severe traumatic injury sometimes caused by rolling wheels or machines. Although avulsed flaps are often readapted to its original site, most of these tissues become necrotic. Due to the extensive skin and soft tissue deficiency caused by necrosis, treatment becomes difficult. Skin grafts harvested from avulsed flaps may be used to treat degloving injuries, while negative pressure wound therapy (NPWT) is used to secure the grafts. Commonly used porous polyurethane foam wound fillers are difficult to set in circumferential extremity degloving injuries; gauze-based wound fillers are easier to use and cause less pain during dressing changes. We present a case of an extensive, full-circumference left lower-extremity degloving injury, treated using NPWT with gauze-based wound fillers for fixation of skin grafts harvested from avulsed flaps after hydrosurgical debridement. For complex wound geometries, gauze-based wound fillers can be easily applied for skin graft immobilization.
INTRODUCTION
Degloving is a severe injury involving avulsion of the skin and subcutis, often caused by rolling machines or wheels, inducing damage to blood vessels, nerves, muscles, and sometimes tendons and bones. Often immediately recovered, avulsed flaps frequently become necrotic, causing an extensive wound which may require several operations and, in some cases, become refractory. Negative pressure wound therapy (NPWT) with porous polyurethane foam wound fillers are sometimes used to secure skin grafts; however, these are unsuitable for degloving injuries. We present a case wherein an extensive and full circumference degloving injury successfully treated with meshed split-thickness skin grafts (STSGs) harvested from the avulsed flaps and fixed by NPWT with a gauze-based wound filler.
CASE REPORT
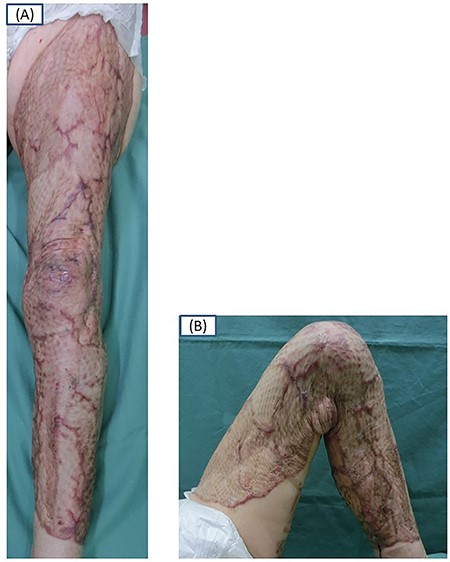
A 79-year-old woman was emergently transferred from a traffic accident site to the emergency center of our hospital with a left lower-extremity degloving injury, sustained when a 10-ton truck had run over her. On admission, the skin and subcutis of the anterolateral part of the left extremity was avulsed as flaps over the fascia; there was extensive injury from the inguinal region to the ankle, with tissue loss on the anterior thigh (Fig. 1). Neither bleeding from the edge nor capillary refilling of the avulsed flap was detected; blood circulation was maintained. The proximal head of the left fibula and right medial and lateral malleoli was fractured; however, the bone fragments were not dislocated. Fractures were treated conservatively and the injury, surgically.

Frontal (A) and oblique (B) views of the left extremity on admission. The anterior and lateral skin and subcutis of the left extremity are avulsed over the fascia and degloved from the inguinal region to the left ankle joint area.
STSGs (all 0.5-mm thick) were harvested from the avulsed skin flaps of the affected leg using an electric dermatome. Additionally, 15 × 5 cm STSGs were harvested from the posterior thigh to cover small defects among the meshed skin grafts. For skin lost on the anterior thigh, a full-thickness skin graft (FTSG) was harvested from the right abdomen using a drum-type dermatome to produce STSG. All grafts were meshed to 5 times the size of the harvested skin; damaged floating subcutaneous tissue was excised.
Debridement was performed using the VERSAJET™ hydrosurgical debridement tool (Smith & Nephew Medical, London, UK) to prepare the wound bed for skin grafting. The total wound area was closed with meshed skin grafts (Fig. 2). Wound dressing material (AQUACEL® Ag BURN, ConvaTec Inc., Flintshire, UK) was placed over these grafts to control infection and secured by NPWT using RENASYS™-G gauze (Smith & Nephew Medical, London, UK) at 120-mmHg continuous pressure (Fig. 3).

Lateral (A) and medial oblique views (B) of the left extremity at grafting. Meshed STSG harvested from the avulsed flap is attached.

An oblique view of the left extremity with wound dressing in place. The meshed skin graft is secured by NPWT set over the wound dressing.
Seven days post-operatively, the skin graft take was confirmed; NPWT was discontinued. The patient reported decreasing pain with successive dressing changes. Eleven days post-operation, surgery was performed on the right medial and lateral malleolus fractures. Two months following operation, the grafts had stably adhered. The knee joint range of motion was 130° on flexion and 0° on extension (Fig. 4), and the patient was able to walk smoothly without aid.
Skin graft take confirmed 2 months after surgery. A frontal view shows the extended knee at 0° (A) and a medial view shows the flexed knee at 130° (B).
DISCUSSION
In this case, the degloving injury was treated with meshed STSGs obtained from the avulsed flap after debridement. Skin grafts taken from the avulsed flap minimized the need for skin from other donor sites, while the VERSAJET™ provided a gentle and adequate depth of debridement. NPWT with RENASYS™-G gauze was easy to perform, resulting in less painful dressing changes and good graft take. The patient’s post-operative course was uneventful, and use of the limb was recovered.
Various procedures have been reported to treat degloving injuries [1, 2]. The musculocutaneous perforators that originally support degloved tissue are often disrupted following injury; thus, revascularization and readaptation of the flap often results in disseminated tissue necrosis [2]. FTSGs from avulsed flaps were initially reported by Farmer in 1939 [3]. In 1952, Innis harvested STSGs from avulsed flaps to treat a degloving injury [4]. Advantages of this approach include lower risk of necrosis, higher possibility of graft success and no or minimal harvesting of skin from donors. Skin graft in degloving injuries makes it possible to cover the open wound, reducing protein and electrolyte loss [5]. In this case, the skin and subcutis were degloved over the fascia, with skin grafts harvested from avulsed flaps.
Successful grafting requires adequate skin graft and wound bed preparation and graft stabilization. Debridement is necessary for preparing both the skin and the wound bed [6], as grossly contaminated injuries have a high risk of infection and worse outcomes for graft take. Debridement may be performed manually or mechanically; however, graft take success is reportedly higher with hydrosurgical debridement than manual debridement [6].
The VERSAJET™ hydrosurgical debridement tool, recently reported to be effective for debridement of necrotic tissue, [6] produces high-quality skin graft defatting and graft-bed preparation via a high-speed stream of saline solution. It thoroughly cleans the wound bed, preventing contamination, preserving healthy tissue and minimizing blood loss [6].
Moreover, stable skin graft fixation contributes to their success. While a tie-over dressing using gauze or cotton is traditionally used, NPWT was recently indicated as an alternative method [2, 7]. NPWT provides firm immobilization, as well as fluid removal, preventing hematoma formation and further contamination, and promoting the growth of granulation tissue and wound blood flow [6, 7, 8]. We performed NPWT instead of traditional tie-over fixation; degloving injuries are generally extensive, and the traditional tie-over dressing technique requires complex operative time and painful dressing changes in cases with significant wound exudate. Conversely, NPWT only requires dressing changes every 2–3 days, which is less stressful for patients [7].
While porous polyurethane foam wound fillers are common for NPWT, gauze-based types are now available [8]. For circumferential injuries of the extremities, foam-type wound fillers are difficult to set for the immobilization of skin grafts, whereas gauze-based types can be more easily applied to complex wound geometries [8]. Moreover, gauze-based NPWT is less painful than foam-based NPWT due to less tissue ingrowth and the non-adherent property of gauze [9, 10]. Gauze-based NPWT is reportedly as efficacious as foam-based NPWT in terms of graft take [8].
We believe that ours is the first report describing the use of gauze-based filler and NPWT for an acute, full circumference degloving injury of the lower extremity. Hydrosurgical debridement and skin graft stabilization by NPWT and gauze-based filler are important to support successful skin graft adherence in severe wounds with irregular geometries.
ACKNOWLEDGEMENTS
We would like to thank Editage (www.editage.com) for English language editing.
FUNDING
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
CONFLICT OF INTEREST STATEMENT
The authors declare that there is no conflict of interest.
CONSENT TO PUBLISH
The patient provided written consent for the publication of data and images.



