-
PDF
- Split View
-
Views
-
Cite
Cite
Curzio Cupellini, Giovanni Alemanno, Andrea Bottari, Annamaria Di Bella, Alessandro Bruscino, Jacopo Martellucci, Carlo Bergamini, Desiree Pantalone, Paolo Prosperi, Laparosacopic management with combination of fatty meal and methylen-blu for chylous leak after a left para-aortic paraganglioma excision, Journal of Surgical Case Reports, Volume 2020, Issue 12, December 2020, rjaa497, https://doi.org/10.1093/jscr/rjaa497
Close - Share Icon Share
Abstract
We report a case of chylous leak recognized post-operatively after abdominal surgery for left para-aortic paraganglioma in a young female with a history of open botallo’s duct. Conservative measures failed to control the leak and the patient is not eligible for sclerotisation. Laparoscopic exploration with intralipidand methylen blue injection through an orogastric tube revealed the leaking area near the superior mesenteric vein behind the Traitz, and this was ligated with non-asorbable suture and placement of acrylic glue. The patient was discharged the 7th post-operative day after removal of the drainage which appeared to supply <100 cc of serum material. Outpatient control was successful and the patient is actually in good conditions.
INTRODUCTION
Demolitive surgery in the retroperitoneal region often requires aggressive dissection which can often lead to injury to the lymphatic ducts or the cisterna chyli [1, 2]. Chylous ascites could be defined as the release of odorless, alkaline, milky liquid with a triglyceride content of more than 200 mg/dl into the abdominal cavity. Usually symptomatology arises subsequently to patient’s re-feeding and is associated to the qualitative and quantitative variation of the surgical drainage (if present), moreover, it could be present progressive abdominal distension and weight loss. Surgery is mandatory when non-operative management or scleroembolization techniques fail.

Patient placement on the operating table. Placed in lateral decubitus position with the affected side elevated around 60°. An optical 10–12 mm trocar is placed on the umbelical line on the left and two 5-mm trocars operating laterally in the left hypochondrion and on the left side on the mid-axillary line.
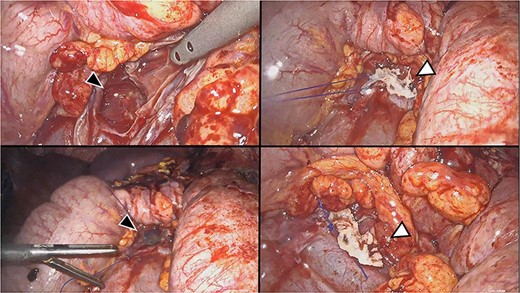
Sequential phases of identification and closure of the leakage. Identification by methylene blue outflow (top black arrow head). Suture with non-absorbable stitch (bottom black arrow head). Cyanoacrylate positioning and final result (respectively, from top to bottom white arrowheads).
This article describes the case of a young patient with aiatrogenic chylous ascites, refractory to medical treatment and not approachable with interventional methodology, which treated effectively with a laparoscopic approach with the combination of fatty meal and methilen-blu.
CASE REPORT
A 32-year-old female, with history of mitral prolapse was submitted to laparoscopic removal of a para-aortic paraganglioma in March 2020. During operation, an extensive mobilization of the left colon and splenic flexure was performed. After the removal of the lesion, a drainage was positioned in the paravertebral site. Re-feeding began on the 1st post-operative day. The day after 1200 cc of odorless, milkyand evocative material for chylous appeared in the surgical drainage. A diet with medium-chain triglyceride (MCT) was undertaken but it was unsuccessful. The patient developed abdominal distension, pain and fever and a CT scan was performed. Blood examination revealed an increase in inflammation indexes (PCR 262 mg/dl, procalcitonin 1.46).
The plan was to consider a lymphoscintigraphy and a radiological interventional treatment with scleroembolization. Patient was submitted to cardiac Ecodoppler that reported an open Botallo’s duct, thus contraindicating the desired interventional procedure. Therefore, it was required to correct lymphatic leakage by surgical operation. On 31st post-operative day, the patient was re-submitted to surgery. A laparoscopic approach was performed positioning the patient on the left flank position, the same used for adrenalectomy.
The previous laparoscopic accesses were used, preparing an optical trocar on the umbilical line on the left side and two operating trocars in the left hypochondrium and left side near the medium axillary line (Fig. 1). To highlight the leak site intraoperatively, a fat meal with methylene blue was administered via NGT at the patient’s induction time. After about 15 minutes, there was a relief of chylous material with traces of blue near the Treitz ligament, cranially at the superior mesenteric vein, but without identifying with certainty the fistulous medium which seemed to be deep in the retroperitoneal zone. It was decided to suture the peritoneal breccia with non-absorbable thread and to tighten it with cyanoacrylate in order to sclerosis the tissues (Fig. 2). At the end, an abdominal drainage was placed in the pelvis.
On the 2nd post-operative day, an MCT feeding was resumed without quantitative or qualitative changes in the surgical drainage. The patient was discharged on the 7th post-operative day after removal of the drainage which appeared to supply <100 cc of serum material. Outpatient control was successful and the patient is actually in good conditions.
DISCUSSION
Therapeutic management of chilous leakage depends on the output. The first therapeutic approach could be conservative and consists in ipo/alipidic diet or total parenteral nutrition in order to reduce the output of chilum and allow a self-repair of the fistula [3, 4]. If conservative treatments fail, could be useful to perform a lymphoscintigraphy, followed by a lympho-embolization of the fistula [5]. When the aforementioned techniques are not applicable, surgical treatment is desirable since chylous ascites is associated with an increase in morbidity, mortality (up to a 65%) and lengthening of hospital stay [1, 3, 6–8].
Diagnosis could be performed with CT scan and chemical analysis of the ascitic fluid. The scleroembolization treatment is a valid option [3–5, 9] even if may cause peripheral emboli and is not applicable in patients with cardiac anomalies.
The laparoscopic approach is a valid therapeutic strategy even if is a technical challenge for surgeons. The recognition of the leak location remains a fundamental point in the treatment of this complications and the administration of fatty meal and methylene blue is easily applicable, helpful and effective, with a rapid waiting time.
Laparoscopy management is preferable to laparotomic approach thanks to the magnification of the lymphatic ducts and represents a valid therapeutic strategy even if requires technical minimally invasive skill.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



