-
PDF
- Split View
-
Views
-
Cite
Cite
Alison M Wallace, George D Oreopoulos, Yoga R Rampersaud, Thomas K Waddell, Three-stage approach to resection of left pancoast tumour with spinal and major vessel involvement, Journal of Surgical Case Reports, Volume 2020, Issue 12, December 2020, rjaa384, https://doi.org/10.1093/jscr/rjaa384
Close - Share Icon Share
Abstract
Here we describe the successful outcome of a complex and challenging resection of a left-sided pancoast tumour involving the left subclavian artery and vertebral bodies. The resection was performed following neoadjuvant chemoradiotherapy in a multi-staged fashion involving multiple teams including thoracic surgery, plastic surgery, neurosurgery and vascular surgery. Each operation was less than 6 h, without complication, and the patient was discharged within 1 week of each procedure. This case report highlights the importance of multidisciplinary team collaboration and planning in order to achieve a successful oncologic outcome and a good quality of life following treatment of these challenging tumours. The patient had a good functional outcome and no evidence of recurrence 1.5 years later.
INTRODUCTION
Pancoast tumours, also known as superior sulcus tumours, are challenging primary lung cancers that arise in the lung apex and invade the surrounding structures [1]. Historically, these tumours were thought to be unresectable, radioresistant and uniformly fatal. Treatment options vary depending on the anatomic site of the lesion, involvement of the surrounding thoracic inlet structures and the presence or absence of distant metastases. Ideally, complete surgical resection is the goal for these patients as complete resection is the most important factor in determining survival [2].
CASE REPORT
An otherwise healthy 59-year-old-male ex-smoker presented with 6 months of left-sided shoulder pain that radiated down the arm and a 30-pound weight loss. He did not have intrinsic hand muscle weakness or Horner’s syndrome [1]. Physical examination and blood tests were normal. MRI to investigate suspected cervical radiculopathy demonstrated a 4.7-cm left upper lobe apical medial tumour invading the T1-T3 vertebral bodies, T1 nerve root and head of the left second rib. The tumour encased the left subclavian artery near its origin (Fig. 1A and B).
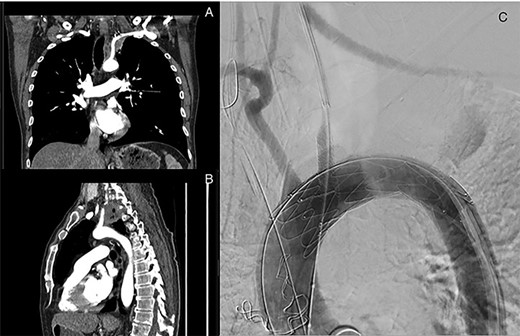
Left superior sulcus tumour encasing the left subclavian artery requiring a left common carotid to subclavian artery bypass and TEVAR placement using in situ fenestration for the left common carotid artery to facilitate resection of the tumour.
A lung biopsy favored squamous differentiation, non-small-cell carcinoma. PET revealed a SUV of 19.3 in the mass but no lymphadenopathy or distant metastases. Brain MRI was negative. Mediastinoscopy was performed to rule out N2 disease and was also negative. Pulmonary function tests were adequate for the planned resection.
Treatment included neoadjuvant chemoradiotherapy with the SWOG protocol (cisplatin with concurrent etoposide) and 60 Gy of radiation over 30 treatments followed by a staged resection [3]. The rationale for giving a radical dose of radiation was to maximize survival outcome in case of disease progression that would limit surgical resection, as well as to improve the pathologic complete response rate and long-term survival [4].
Preoperative planning involved multi-disciplinary consultation among thoracic, vascular, spinal and plastic surgical teams, as well as interventional radiology. A three-stage approach was planned that involved vascular isolation, followed by a posterior approach for spinal mobilization and instrumentation and then finally en-bloc resection of the tumour. Operative staging was designed to optimize radiographic imaging during vascular tumour isolation prior to spinal instrumentation. Prevention of erosion of the spinal hardware into vital structures was also considered imperative.
The first stage involved a left hemi-clamshell incision with neck extension, osteotomy with first rib resection, left carotid-subclavian bypass with 6-mm Dacron graft and TEVAR placement using in situ fenestration for the left common carotid artery to facilitate resection of the tumour off the aorta (Fig. 1C).
One week later, the second stage was undertaken through a posterior approach. This involved an en-bloc resection of the T1-T3 spinal elements; laminectomy from C7-T4; ligation of left T1-T3 nerve roots; dissection of the posterolateral chest wall bilaterally and release of the upper first rib with transection of the rib lateral to the transverse processes and lung margin, as well as harvesting of 8 cm of the sixth rib from the left chest wall; and stabilization from C2-T7.
Ten days following this, stage three was completed. The previous anterior incision was reopened. A pectoralis muscle flap was created with care to preserve the thoracoacromial vessel pedicle. The patient underwent en-bloc resection of the left upper lobe, the posterior aspects of ribs 1–3 and the vertebral bodies of T1-T3; division of the subclavian artery at its origin; ligation of the vertebral artery; exploration of the brachial plexus; spinal column reconstruction and pectoralis muscle flap insertion between the spinal instrumentation and mediastinal structures to prevent erosion. The patient also received five hyperbaric oxygen sessions postoperatively in order to prevent breakdown and infection of the surgical wound as this would potentially compromise the vascular graft and spinal hardware. The patient suffered no major complications or stroke and was discharged home on postoperative day 7.
The final pathology showed an invasive keratinizing squamous cell carcinoma, ypT3 N0, with less than 10% residual viable tumour. Resection margins were all negative, the closest being 0.2 cm from the lateral soft tissue near the subclavian artery. All seven sampled lymph nodes were negative. LVI was present. PD-L1 was 2%.
With regards to further treatment, the PACIFIC clinical trial showed that with definitive chemoradiation adding durvalumab for 1 year improves 3-year overall survival [5]. However, the PACIFIC trial did not involve surgical resection. Therefore, the benefit of adding durvalumab was unclear and we did not to proceed with durvalumab in this case.
DISCUSSION
This trimodality treatment plan with a three-stage, multidisciplinary operative approach enabled successful resection of this complex pancoast tumour and good biologic response to chemoradiation. We believe the key points in this case were performing endovascular isolation prior to the spinal instrumentation to achieve clear visualization, as well as placement of a muscle flap between the mediastinal structures and spinal hardware to prevent future complications such as erosion into the esophagus or major vascular structures that we had experienced with a previous patient. The patient is now 2 years out from surgery. There is no evidence of recurrence on serial imaging and functionally he is doing well with minimal neurologic deficits.



