-
PDF
- Split View
-
Views
-
Cite
Cite
Nicole Reyes, Lauren E Smith, David Bruce, Strangulated internal hernia due to defect in broad ligament: a case report, Journal of Surgical Case Reports, Volume 2020, Issue 11, November 2020, rjaa487, https://doi.org/10.1093/jscr/rjaa487
Close - Share Icon Share
Abstract
Small bowel obstruction is a relatively common disease process accounting for up to 16 percent of surgical admissions and more than 300,000 operations annually in the United States. Approximately 5–8 percent of small bowel obstructions can be attributed to internal hernias. A slightly lower percentage, roughly 4–7 percent, of these internal hernias are noted to originate from a defect in the broad ligament of the uterus. A majority of broad ligaments defects causing a small bowel obstruction are not diagnosed preoperatively due to the equivocal imaging findings as well as the infrequency of this etiology. To date, there are very few case reports describing this disease process. This case report describes a 70-year-old female who was found to have a defect in her broad ligament causing a small bowel obstruction leading to subsequent strangulated bowel.
INTRODUCTION
Small bowel obstruction is a common disease process accounting for up to 16 percent of surgical admissions and 300,000 operations annually in the United States [1]. Approximately 5–8 percent of small bowel obstructions can be attributed to internal hernias [2]. A small percentage of these internal hernias are noted to originate from a defect in the broad ligament of the uterus [3]. In 1861, Quain documented the first known case of a broad ligament hernia. He reported autopsy findings in a woman who died of intestinal obstruction by strangulation in an opening of the right broad ligament [4]. Broad ligaments defects causing a small bowel obstruction are difficult to diagnose preoperatively due to the equivocal imaging findings as well as rarity of this etiology. To date, there are few case reports describing this disease process. This case report describes a 70-year-old female who was found to have a defect in her broad ligament causing a small bowel obstruction leading to subsequent strangulated bowel.
CASE REPORT
A 70-year-old female presented to the ER complaining of sharp suprapubic abdominal pain of six hours duration. She denied any fever, chills, nausea, or vomiting. Her past medical history was significant for hypertension and osteoporosis. Her past surgical history included: laparoscopic sleeve gastrectomy, tubal ligation, and a total right hip replacement. She took Triamterene-Hydrochlorothiazide 37.5–25 mg and a multivitamin daily.
On physical exam, she was afebrile and normotensive. Her abdomen was soft with tenderness to palpation in the suprapubic region. Laboratory data demonstrated a white blood count of 7,200, a hemoglobin of 13.2, and a hematocrit of 39.3 percent. Renal function, electrolytes, liver function, and urinalysis were all within normal ranges. A CT of the abdomen and pelvis with intravenous contrast was obtained and revealed distended fluid-filled loops of small bowel mostly within the pelvis. There was evidence of some wall thickening and perienteric fat stranding. A transition point was felt to be within the pelvis (Figs 1 and 2).
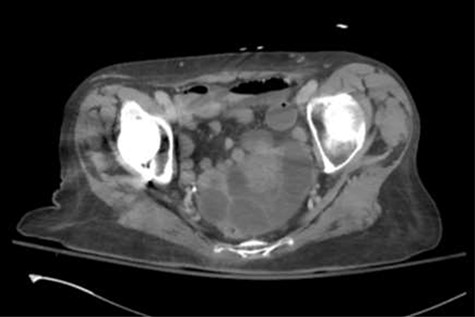
Axial slice of the CT of the abdomen/pelvis demonstrating distended fluid-filled loops of small bowel mostly within the pelvis. There was evidence of some bowel wall thickening and perienteric fat stranding.

Coronal slice of the CT of the abdomen/pelvis demonstrating distended fluid-filled loops of small bowel mostly within the pelvis. The transition point was identified in the pelvis.
Due to the above findings yet overall benign physical exam, the patient was presented with the options of conservative nonoperative management versus operative management. She elected to undergo a trial of conservative nonoperative management. She was admitted to the hospital, kept NPO, and resuscitated with intravenous fluids.
Forty-eight hours after admission, the patient remained afebrile and her vital signs were stable within a normal range. However, she exhibited a significant increase in her white blood cell count to 19,700. Her renal function, electrolytes, and liver function remained within normal limits. She continued to complain of suprapubic abdominal pain. There was concern that the patient was not progressing via a conservative treatment approach; therefore, the decision was made to take the patient to the operating room for a diagnostic laparoscopy.
Once in the abdomen, significant distension of the patient’s small bowel was noted. This created difficulty with safe visualization; therefore, the procedure was converted to an exploratory laparotomy. A full inspection of the abdominal contents was completed. There was evidence of a defect within the left side of the patient’s broad ligament (Fig. 3). A portion of the patient’s small bowel had herniated through this defect thus creating a strangulated internal hernia. The contents of the hernia were fully reduced and a small bowel resection was performed due to the ischemic nature of that portion of the bowel. A left salpingoophorectomy was also performed in order to eliminate the internal hernia defect.
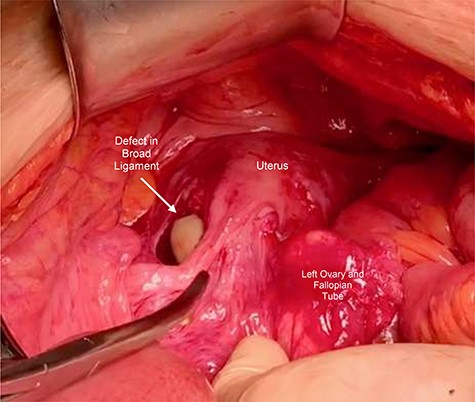
Intraoperative photograph of a defect within left side of broad ligament. The left ovary and fallopian tube have been reflected medially.
The patient did well post-operatively and she was discharged home four days after surgery. The patient unfortunately returned to the emergency room and was readmitted to the hospital on post-operative day 12 due to complications with COVID-19 infection. She continued to do well from a surgical standpoint.
Discussion
In the United States, a majority of small bowel obstructions are caused from adhesive disease after abdominal surgery [1]. About 65–80 percent of patients will respond to conservative treatment which includes bowel rest, nasogastric tube decompression, and serial abdominal exams. However, approximately 24 percent of patients will fail this treatment pathway [5]. The majority of small bowel obstructions secondary to internal hernias fall into this category.
Without surgical intervention, the mortality rate of strangulated internal hernias approaches 100 percent [3]. Unfortunately, a big challenge is the ability to diagnose internal hernias in the preoperative setting. The typical woman presenting with a broad ligament hernia is one that is middle-aged and multi-parous [6, 7]. Some case reports have described certain CT findings that may suggest the diagnosis of a broad ligament hernia leading to a small bowel obstruction; these findings may include a closed-loop obstruction with a double transition zone in the pelvis, a cluster of dilated small bowel loops herniated laterally to the uterus, enlargement of the distance between the uterus and ovary deviating in opposite directions, and displacement of the uterus to the opposite side [2, 6, 7].
Some theories exist about the etiology of broad ligament defects. They can be categorized into congenital versus acquired. Congenital defects arise from spontaneous rupture of congenital cystic structures within the broad ligament reminiscent of the mesonephric or Mullerian ducts [8]. On the other hand, acquired defects can originate from operative trauma, delivery trauma, endometriosis, or previous pelvic inflammatory disease [9, 10].
Ultimately, this case serves three important lessons: First, to remind us, as diagnosticians, to maintain an open mind when a relatively common problem presents itself. Second, to help raise awareness that even if the common CT findings associated with internal hernias of the broad ligament are not visualized, this rare hernia cannot be entirely ruled out. And third, that if incidentally found, broad ligament defects warrant repair to help prevent future complications.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
ETHICAL APPROVAL
Ethical approval from the Kettering Health Network institutional review board was obtained (IRB# 1666268–1).
CONSENT
Consent from the patient for this case report was obtained.



