-
PDF
- Split View
-
Views
-
Cite
Cite
Yunchong Meng, Han Xiao, Zheng Zhang, Kuo Li, Quanfu Huang, Wenlin Qiu, Yongde Liao, Minimally invasive esophagectomy with intrathoracic anastomosis in a situs inversus totalis patient, Journal of Surgical Case Reports, Volume 2020, Issue 11, November 2020, rjaa480, https://doi.org/10.1093/jscr/rjaa480
Close - Share Icon Share
Abstract
Situs inversus totalis (SIT) is a rare congenital condition, which is characterized by abnormal placement of the thoracic and abdominal organs. The incidence of this condition is estimated to be from 1/8000 to 1/25,000. There have been minimal reports on SIT patients with esophageal cancer. In this report, we discuss a patient with SIT complicated by middle and lower esophageal cancer who underwent laparoscopic and thoracoscopic esophagectomy with intrathoracic anastomosis, and provide useful information with regards to treatment of this rare condition.
INTRODUCTION
Situs inversus is a rare congenital disease characterized by the abnormal arrangement of organs in the thorax and abdomen. This condition can be divided into complete situs inversus, known as situs inversus totalis (SIT), and incomplete situs inversus [1]. Arranged in a mirror image of their usual positions, the organs of SIT patients are completely transposed in a right-to-left reversal. SIT is rare, and SIT patients with esophageal cancer are rarer still [2]. To date, intrathoracic anastomosis in conjunction with a minimally invasive esophagectomy of an SIT patient has been reported only once [3]. Here, we discuss an SIT patient whose condition was complicated by middle and lower esophageal cancer. This patient underwent laparoscopic and thoracoscopic esophagectomy with intrathoracic anastomosis.
CASE REPORT
A 55-year-old man was admitted to hospital with progressive dysphagia. The patient was found to have mirror-image dextrocardia (Fig. 1) with an abnormally thickened esophageal wall (thoracic middle-lower segment) observed by way of contrast-enhanced computed tomography (CT) of the chest (Fig. 2a). SIT was observed in the patient, with a right-sided position of the heart and aortic arch (Fig. 2b). Additionally, the spleen and stomach were observed on the right side and the liver on the left by means of CT of the upper abdomen (Fig. 2c). Based on the preoperative examination, the patient was diagnosed with esophageal carcinoma, which was clinically staged as T3N0M0, stage IIA (Union for International Cancer Control esophageal carcinoma pathological stage, 2017). Laparoscopic and thoracoscopic esophagectomy with intrathoracic anastomosis was determined to be the best treatment for the patient’s middle-lower esophageal carcinoma. Throughout the laparoscopy-assisted abdominal surgery, the patient was placed in a supine position. The surgeon stood on the left side of the patient, which is the opposite of the standard position. Under the laparoscope, in accordance with preoperative imaging, the stomach was observed in the right hypochondriac region, the spleen to the right and rear of the stomach, and the liver on

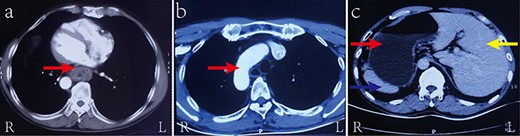
Contrast-enhanced CT of the chest and upper abdomen showing (a) the abnormally thickened esophageal wall of the thoracic middle-lower segment (red arrow); (b) the aortic arch as arranged in SIT (red arrow); and (c) the liver (yellow arrow), stomach (red arrow), and spleen (blue arrow) as arranged in SIT

Intraoperative observation demonstrating (a) the stomach (red arrow) in the right hypochondriac region, the spleen (blue arrow) on the right rear of the stomach, and the liver (yellow arrow) on the left; (b) the azygos vein (blue arrow) and the three lobes (red arrow) in the left thoracic cavity; and (c) the esophageal carcinoma (red arrow)
the left (Fig. 3a). The patient’s stomach was routinely mobilized, the abdominal lymph node was dissected, and the anastomosis was circularly embedded with the pedicled omentum flap. An assistant abdominal incision was subsequently made below the xiphoid process, and a gastric conduit of ~3.5 cm in diameter was created using a linear stapler outside the abdominal cavity.
Before the two-port thoracoscopy-assisted thoracic surgery began, the patient was repositioned in a right prone position. The surgeon stood on the abdominal side of the patient. Intraoperative observation revealed that the azygos vein and the three lobes lay in the left thoracic cavity (Fig. 3b). A tumor 5 cm in length with a maximum diameter of 3 cm was located in the middle and lower segment of the esophagus (from 2 cm above inferior pulmonary vein to 2 cm above the diaphragm) (Fig. 3c). The esophagus was mobilized at a site 4 cm superior to the azygos vein, and the pleura surrounding the esophagus at the anastomotic stoma and thoracic lymph nodes were systematically dissected. The remaining steps in this surgery resembled that of surgery performed on situs solitus patients with esophageal cancer and consisted of purse-string suturing, the insertion of the anvil of the stapler, distal esophagectomy, and intrathoracic anastomosis of the esophageal stump and the tubular stomach.
The overall operation time was 270 minutes, and estimated blood loss was 150 ml. Postoperative pathology confirmed that a well to moderately differentiated squamous cell carcinoma classified as T3N1M0 stage IIIB. There were no postoperative complications such as trachyphonia or other symptoms related to recurrent laryngeal nerve injury.
DISCUSSION
A rare autosomal recessive disease, SIT was first described in 1600 by Fabricius [4], and its incidence ranges from 1/8000 to 1/25,000 in the general population [5]. Other than their anomalous organ arrangement, most SIT patients have relatively normal anatomy. However, 20–30% of SIT cases coexist with Kartagener syndrome, which is characterized by a triad of conditions: bronchiectasis, sinusitis or nasal polyps, and situs inversus. In clinical practice, we rarely encounter a case of esophageal cancer complicated by SIT. The surgical treatment of esophageal cancer has evolved from traditional open surgery to minimally invasive surgery. Yoshida et al. [6] first reported a patient with SIT underwent simultaneous hand-assisted laparoscopic gastric mobilization and thoracoscopic esophagectomy in 2004. Later, other case reports followed, with cervical anastomosis used in most of cases [2, 7–8]. Intrathoracic anastomosis was reported only once [3]. This 2014 study by Peel et al, however, did not focus on surgical techniques, but rather on the treatment of SIT in Kartagener syndrome. In our case, intrathoracic anastomosis was selected instead of cervical anastomosis to achieve radial resection of the nidus and decrease the incidence of severe complications such as recurrent laryngeal nerve injury and anastomotic leak. This surgical method is technically feasible and secure [9].
There are two predominant reasons why the presence of SIT can complicate surgeries. One is that the anomalous translocation of viscera that occurs in SIT requires a surgical team to be flexible and accommodate this reversal of organs by performing surgery in a mirror image of what it would be under normal circumstances. As described above, this was reflected in the positioning of the patient, respiratory management, endoscope incisions, mobilization of the organs, lymph node dissection, et cetera. Fortunately, the relative anatomical position of organs in most SIT patients is the same as that in situs solitus patients, which decreases the difficulty of thoracoscopic and laparoscopic surgery and ameliorates the risks involved. Another reason SIT increases the difficulty level of these surgeries is that SIT patients often have comorbid conditions, for example Kartagener syndrome. In our case, Kartagener syndrome was not found. Patients with Kartagener syndrome often have respiratory infections due to poor mucociliary clearance, especially in surgical conditions. Complete preoperative examination, including necessary imaging and cardiopulmonary function assessment, and careful perioperative management of respiratory tract are therefore vital to avoiding severe postoperative complications such as sepsis and respiratory failure.
CONSENT
Written informed consent was obtained from the patient for publication of this manuscript.
CONFLICT OF INTEREST STATEMENT
None declared.
Funding
None.
References
Author notes
Yunchong Meng and Han Xiao contributed equally to this work.



