-
PDF
- Split View
-
Views
-
Cite
Cite
Luke Geoghegan, Billie-Georgina Knowles, Dariush Nikkhah, A patient with chronic fingertip pain, Journal of Surgical Case Reports, Volume 2020, Issue 11, November 2020, rjaa477, https://doi.org/10.1093/jscr/rjaa477
Close - Share Icon Share
Abstract
Isolated chronic fingertip pain is an uncommon presentation with a broad differential diagnosis, including but not limited to, subungal neuroma, subungal haematoma, subungal exostosis and glomus tumour. We present an interesting case of a young lady with debilitating chronic fingertip pain diagnosed with a glomus tumour of her right index finger. Surgical excision provided complete resolution from pain, return to work and restoration of quality of life. Here we discuss clinical and radiological features of this rare benign neoplasm.
INTRODUCTION
A glomus body is a peripheral neurovascular structure comprising an arteriovenous shunt surrounded by perivascular smooth muscle cells [1]. The glomus body functions to maintain skin temperature through vasodilation and vasoconstriction in response to warm and cold ambient temperature respectively. Glomus bodies are located throughout the stratum reticulare of the dermis although they are highly concentrated in the subungual region of the digits (Fig. 1). Glomus tumours are benign neoplasms of the glomus body. Although the exact incidence of glomus tumour is unknown, 75% are subungual in location and they account for between 1 to 5% of all soft tissue tumours affecting the hand [2]. Here we present an interesting case of glomus tumour affecting the dominant index finger of a young, otherwise well female and discuss key clinical and radiological findings that aid in the diagnosis of this debilitating and readily treatable condition.
CASE REPORT
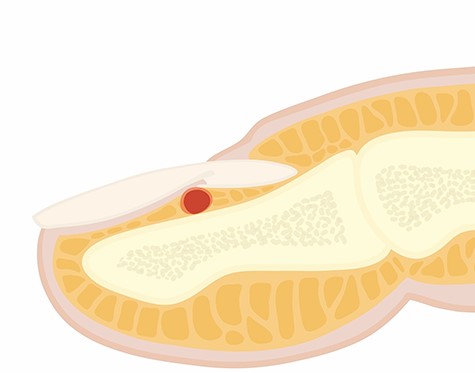
A 41-year-old right hand dominant female presented to the hand surgery clinic with 4-year history of fingertip pain affecting her right index finger, which significantly impaired hand function. She had an unremarkable past medical history and works as an administrator. On examination there were no visible deformities with preserved range of motion throughout the distal and proximal interphalangeal joints as well as the metacarpal phalangeal joints. On closer inspection, there was a violaceous hue noted on the nail plate (Fig. 2). Fingertip pain was intensified following application of pressure via a pin head and the patient reported a reduction in pain following application of a digital tourniquet. A radiograph of the affected digit demonstrated no bony abnormalities. Ultrasonography of the distal phalanx demonstrated a discrete mass measuring 0.4 by 0.6 cm on the dorsal aspect of the distal phalanx and a glomus tumour was subsequently diagnosed. The patient underwent excision of the glomus tumour by raising an eponychial flap and removing the tumour through a transungal approach (Fig. 3). Surgical excision provided complete pain relief and subsequent significant improvement in perceived hand function.

Pre-operative clinical photograph demonstrating violaceous hue of the nail plate.

Intra-operative photograph demonstrating a well circumscribed lesion of the glomus body.
DISCUSSION
Glomus tumour can be distinguished from other causes of fingertip tenderness through the cold sensitivity, Love’s pinpoint and Hildreth’s tests. The cold sensitivity test has a reported sensitivity and specificity 100% for glomus tumour with intensification of pain following digital submersion in cold water. Love’s pinpoint test is performed by application of pressure classically using the round head of a metal pin, withdrawal of the affected digit secondary to pain has a reported 100% sensitivity and specificity for glomus tumour [3]. Hildreth’s test is positive if pain is alleviated following application of a digital tourniquet. It has a reported sensitivity of 77.4% and specificity of 100% in glomus tumour [3]. The classic triad of pain, temperature sensitivity and point tenderness is non-specific and may not be present [4].
Plain radiograph reveals a lytic lesion on the dorsal aspect of the distal phalanx in 36% of cases [5] and ultrasonography may demonstrate a well circumscribed lesion on the dorsal aspect of the distal phalanx. High resolution MRI with hyperintensity on T2-weighted imaging demonstrates pseudocapsule formation due to local inflammatory processes and has a 90% sensitivity, 50% specificity, 97% positive predictive value and 20% negative predictive value in the diagnosis of glomus tumours [6].
Surgical excision is the treatment of choice either directly through the nail via a trans-ungual approach or through a lateral subungual or lateral subperiosteal approach which does not penetrate through the nail proper. The lateral sub-periosteal approach is generally preferred as reduces the risk of nail deformity. Elevation in the sub-periosteal plane creates a composite dorsal flap containing all neurovascular structures dorsal to the phalanx [7]. Subungual structures can be easily visualized and resected, the adjunctive use of an operative microscope may be necessary to ensure complete resection [8]. Excellent long-term outcomes have been reported following prompt diagnosis and excision. Santhoshi et al. [9] report complete resolution of symptoms in 97% of patients (36/37) at 6-months post excision. A further case report by Altinel et al. [10] demonstrated comparable outcomes at 6 months with complete resolution of pain, no recurrence or nail deformity following a transungual resection. Vasisht [7] reported complications in 10% of patients (2/19, one paronychia and one temporary nail loss) with a 15.7% recurrence rate (3/19).
In conclusion, glomus tumour is a rare but readily treatable cause of chronic fingertip pain which should be evaluated for in the clinical setting using the cold sensitivity, Love’s pinpoint and Hildreth’s tests alongside diagnostic imaging studies. Further long-term follow-up studies reporting recurrence, hand function and condition specific patient reported outcome measures following excision are required.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



