-
PDF
- Split View
-
Views
-
Cite
Cite
Orgeness J Mbwambo, Alex Mremi, Jasper S Mbwambo, Frank Bright, Alfred K Mteta, Bartholomeo N Ngowi, Virchow’s node as the initial presentation of metastatic prostate cancer: a case series of a common cancer in uncommon location, Journal of Surgical Case Reports, Volume 2020, Issue 11, November 2020, rjaa476, https://doi.org/10.1093/jscr/rjaa476
Close - Share Icon Share
Abstract
Prostate cancer is one of the commonest cancers among men contributing significantly to the overall cancer burden globally. Most patients present with lower urinary tract symptoms. Metastasis to supraclavicular lymph nodes is unusual presentation, which has been rarely reported particularly as the primary presentation. We report two rare cases of advanced prostatic adenocarcinoma presenting with firm, non-tender lump in the left supraclavicular region between the two heads of the sternocleidomastoid muscle, (that is Virchow’s node) as initial primary symptom. Examination of the patients revealed an elevated prostatic-specific antigen (PSA) of > 100 ng/ml levels, and the diagnosis was confirmed by histological evaluation and immunostaining with PSA of the supraclavicular lymph nodes and prostate biopsies. This case series emphasizes the importance of considering prostate cancer in the differential diagnosis of male patients with supraclavicular lymphadenopathy.
INTRODUCTION
Prostate cancer is one of the most common cancers affecting males with adenocarcinoma being the most common histological type accounting for >90% [1]. The clinical presentation varies widely from asymptomatic early disease to metastatic symptoms. Regional lymph node is the most common site of metastasis, other sites includes skeletal and lungs. Metastasis to non-regional supraclavicular lymph node has been documented but is extremely rare presentation of prostate cancer [1, 2]. Among the few cases of supraclavicular lymph node metastasis reported, left supraclavicular node is the most common site [2]. Neck lymph node is common site for metastasis of malignances of head and neck [1]. Other primary cancers that rarely metastasize to cervical nodes include kidney, lung and breast [3]. African patients are likely to present with more advanced disease compared to Caucasians [4]. We report two rare cases of prostate cancer that presented initially with asymptomatic left supraclavicular swelling.
CASE SERIES
Case number 1
An 80-year-old male presented with left supraclavicular swelling, which was started gradually. The swelling was painless, progressively increasing over time. He attended at a local health facility where a supraclavicular lymph node incisional biopsy was done, and the histopathology report suggested the diagnosis of metastatic adenocarcinoma, most likely from the prostate. The patient also reported lower urinary tract symptoms, which were characterized by urgency, weak stream, straining and increased frequency of micturition. These symptoms were associated with lower back pain; however, there was no aggravating or relieving factor. He denied history of blood in urine, prior trauma on his back, weakness of the lower limbs, loss of consciousness, headaches or difficulties in breathing or swallowing.
The patient was then transferred to our facility for further management. There, the patients reported that he was apparently well until 6 months ago when he started to experience lower urinary tract symptoms, which included urgency, weak stream, straining, sensation of incomplete bladder emptying, hesitancy, intermittency and increased frequency of micturition both during day and night time. However, he denied the history of blood in urine. On physical examination, he was fully conscious; his vital signs were all within normal limits. A transverse incision scar associated with a 3 × 4 cm, firm, non-tender lump with irregular surface in the left supraclavicular region between the two heads of the sternocleidomastoid muscle was noted. There was no any other peripheral lymph node enlargement. Abdominal examination revealed no organomegaly, no palpable masses. Digital rectal examination revealed hard, nodular prostate on both lobes with obliteration of median sulcus. Other systems examination was unremarkable.
Abdominal pelvic ultrasound showed right moderate hydronephrosis with multiple pelvic masses that were separate from heterogeneous prostatomegaly (Fig. 1A). Kidney, ureter and bladder (KUB) X-ray revealed multiple osteoblastic lesions on the iliac wings and lumbar vertebrae (Fig. 1B); however, chest X-ray was normal (Fig. 1C). Abdominopelvis computed tomography scan was ordered but due to financial constraints, the patient was unable to afford, thus the staging was done by combination of the clinical presentation of the patient; (T3) as the prostate capsule was hard with an extra-capsular extension; (N3) due to the presence of supraclavicular lymph node involvement and (M1a) for the presence of osteoblastic lesions on the bone from the X-ray (Fig. 1C).

Ultrasound showing pelvic masses (A), kidney, ureter and urinary bladder X-ray showing osteoblastic lesions (B), and normal chest X-ray (C)
Total serum prostate-specific antigen (PSA) was > 120 ng/ml (normal range 0.001–4.000). Urinalysis showed 15-20 wbc/hpf (normal range 0–5 wbc/hpf), other parameters were normal. Complete blood count, random blood sugar and serum creatinine were within normal range.
Transurethral resection of prostate and supraclavicular lymph node excision biopsies were done whose histopathology results revealed invasive adenocarcinoma of the prostate, Gleason score 4 + 5 = 9 (Fig. 2A), with supraclavicular node involvement (Fig. 2B). Further, with appropriate control, the tumor cells in the supraclavicular lymph node stained positive for PSA immunostaining (Fig. 3).
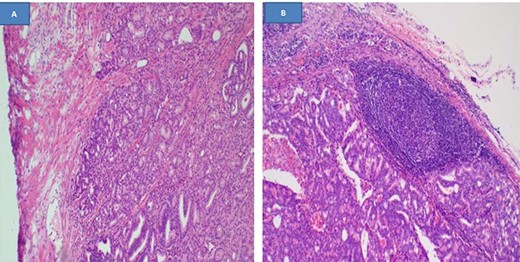
Histopathology demonstrating invasive prostatic adenocarcinoma, hematoxylin and eosin staining x40 (A), and a lymph node infiltrated by prostatic adenocarcinoma, hematoxylin and eosin staining x100, (B)
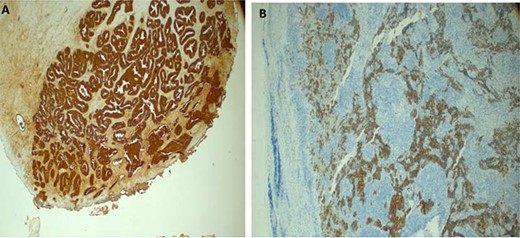
Immunostaining of the supraclavicular lymph node with (PSA highlighting tumor cell positivity, immunohistochemstiry (IHC) x40 in prostate biopsy (A) and supraclavicular lymph node, IHC x20 (B)
A month later, the patient underwent surgical androgen deprivation therapy (ADT) with bilateral total orchiectomy and later kept on chemotherapy including casodex. The lymph node regressed significantly and clinically the patient was stable in the subsequent follow-ups with decreasing serum PSA level and free from obstructive uropathy symptoms.
Case number 2
A 73-year-old male who presented to us with history of swelling on left side of neck for 3 months following a 4-month history of lower urinary tract symptoms. The swelling was painless, started gradually and progressively increased in size over time. However, he denied history of hematuria, loss of consciousness, headache and difficulties in swallowing or breathing.
On general examination he was fully conscious, oriented to time place and people, pale, multiple masses on the left supraclavicular area that were mobile, the largest measured 4 × 5 cm. The rest of the peripheral lymph nodes were not palpable.
Abdominal examination was unremarkable. On digital rectal examination, the prostate was irregular and both lobes were hard. Other systems were unremarkable. Hemoglobin level was 9.6 gm/dl, serum creatinine was 1.35 mg/dl, and total serum PSA was > 120 ng/ml.
Abdominal ultrasound revealed ill-defined, heterogeneous prostate and paraaortic lymph nodes enlargement. The rest of the abdomen was normal. Ultrasound of the neck showed multiple left supraclavicular hypodense well-marginated masses with hyper vascularity. The largest mass was approximately 4.21 × 4.45 cm (Fig. 4A). KUB X-ray revealed extensive osteoblastic lesions involving the lumbosacral spine, pelvic bone and proximal part of the femur bilaterally (Fig. 4B). Chest X-ray was negative for metastasis (Fig. 4C).

Ultrasound of left neck showing supraclavicular mass (A), kidney, ureter and urinary bladder X-ray showing extensive osteoblastic lesions (B) and normal chest X-ray (C)
He underwent channel transurethral resection of prostate and left supraclavicular lymph node excision biopsy. Histology results confirmed the diagnosis of prostatic adenocarcinoma, Gleason score 5 + 4 = 9; group grade 5 (Fig. 5A) with supraclavicular lymph node involvement (Fig. 5B). He was doing fine postoperatively. He was counseled for ADT but unfortunately he succumbed shortly before initiation of the treatment due to sepsis.
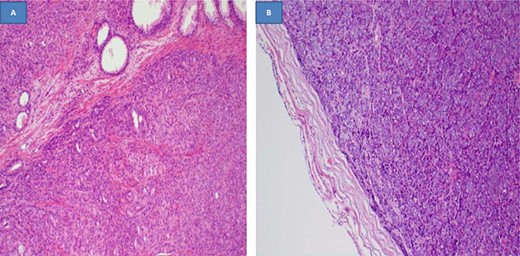
Histopathology of the prostate tissue showing invasive adenocarcinoma, hematoxylin and eosin staining x100 (A), and a lymph node with complete effacement and replaced by a solid tumor, hematoxylin and eosin staining x100 (B)
DISCUSSION
Prostate cancer is one of the most common cancers affecting elderly men worldwide [1]. Metastatic prostate cancer to the left supraclavicular region between the two heads of the sternocleidomastoid muscle, that is, Virchow’s node is a rare presentation accounting for about 0.28% [4]. Virchow’s node lies near to the junction of the thoracic duct and the left subclavian vein, where the lymph from most of the body drains into the systemic circulation [5]. The route of spread is thought to involve regional lymph nodes, retroperitoneum, cysterna chili, thoracic duct sequentially and finally to left supraclavicular lymph nodes [5]. Hematogenous spread through the Batson plexus fails to explain the predilection to supraclavicular lymph nodes [5].
In America, African–American males have a slightly higher incidence and mortality rates of prostate cancer than Caucasian males. In the case reports by Ahamed et al. [4] and Woo et al. [6], both patients presented with high PSA levels of 586 and 326 ng/ml, which suggest an aggressive cancer. In a case series of 19 patients of prostate cancer with supraclavicular metastasis by Butler et al. [7], only 42% of patients presented with abnormal digital rectal examination, whereas Cho et al. [8] reported 26 cases of metastatic prostatic carcinoma in supradiaphragmatic lymph nodes from 1972–87 of which 15 were supraclavicular, 8 were cervical, 2 were axillary, and 1 was mediastinal. Among their patients, 84.6% had high Gleason score and 76% of patients had abnormal levels of PSA [8].
In a case report of an African American by Jain et al. [9], the patient presented with aggressive disease (marked elevated PSA, metastasis to the bone, bulky retroperitoneal lymphadenopathy, mediastinal lymphadenopathy and obstructive renal failure) similar aggressive clinical behavior was the case to our patients. The most significant predictor of mortality in prostatic adenocarcinoma is the presence of distant metastases. The prognosis for prostate cancer with supraclavicular metastasis is known to be poor; however, some of case series reported no progression during follow-up after initiation of hormonal therapy [8, 9].From our two cases, both patients presented with high PSA levels, high Gleason score and bone metastasis, which suggest an aggressive cancer behavior. Studies comparing the prognosis of prostate cancer patients presenting with supraclavicular lymph node metastasis and those without supraclavicular lymph node metastasis are limited. Long-term follow-up of this rare group of patient in native Africans is needed to assess if it is different from other patients who present with metastatic disease such as lumbosacral osteoblastic lesions. Furthermore, high index of suspicion of prostate cancer is needed among clinicians particularly when elderly male patients present with supraclavicular lymph nodes, as may indicate a metastatic prostate cancer presenting with a Virchow’s node [7–10].
From the two cases, we have learnt that it is important to have a high index of suspicion for metastatic prostate cancer in male patients presenting clinically with Virchow’s node with or without other signs and symptoms as in our cases despite of the wide spectrum of the potential differential diagnoses. Special staining with prostate cancer markers, like PSA and PAP are useful to rule out the potential differentials for metastatic prostate cancer and thus making a definitive diagnosis.
ACKNOWLEDGMENTS
We extend our sincere thanks to the patients who consented for the study, urology, medical records and pathology departments staffs for their assistance in getting the patients information.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
A written informed consent to undergo treatment including surgery and chemotherapy as well as to use de-identified patient’s data for academic purposes for publication was obtained from both patients. Copies are available for review if requested by editorial office.
CONSENT FOR PUBLICATION
The consent for publication was obtained along with an informed consent from the patients.
AVAILABILITY OF DATA AND MATERIALS
All the information included in the current study is available from the corresponding author upon editorial office’s special request.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
References
- immunohistochemistry
- cancer
- adenocarcinoma
- antigens
- differential diagnosis
- neoplasm metastasis
- prostate-specific antigen
- diagnosis
- prostate
- metastatic prostate cancer
- prostate cancer
- prostate biopsy
- virchow's node
- sternocleidomastoid muscle
- lower urinary tract symptoms
- supraclavicular lymph node
- supraclavicular lymphadenopathy
- supraclavicular region of neck



