-
PDF
- Split View
-
Views
-
Cite
Cite
Victor Gazivoda, Lawrence P Kiss, Rebecca Rhee, A rare case of perianal apocrine adenocarcinoma, Journal of Surgical Case Reports, Volume 2020, Issue 11, November 2020, rjaa463, https://doi.org/10.1093/jscr/rjaa463
Close - Share Icon Share
Abstract
Apocrine adenocarcinoma is a rare primary cutaneous malignancy that arises from areas with high apocrine gland density, most frequently described in the axilla. There have only been three previously reported cases of apocrine adenocarcinoma in the anal/perianal region. A 72-year-old female presented for evaluation of a perianal lesion with persistent drainage that she had noticed for over a year. The patient proceeded with surgical excision of the perianal nodule. Diagnosis was made based on pathology demonstrating areas of mixed solid and trabecular areas with large nuclei and many prominent mitotic figures, which stained positive for periodic acid–Schiff–diastase, cytokeratin 7 and gross cystic disease fluid protein 15. We are reporting just the fourth such case of apocrine adenocarcinoma in the anal/perianal region. It is important to consider apocrine adenocarcinoma in our differential, because though apocrine adenocarcinoma has a benign clinical presentation, it can have a high incidence of lymph invasion on presentation.
INTRODUCTION
Apocrine adenocarcinoma is a rare primary cutaneous malignancy that has mostly been described in case reports and case series. They primarily arise from areas with high apocrine gland density, most frequently described in the axillary region [1]. They have also been described in regions of the scalp, ear canal, eyelids (Moll’s gland carcinoma), chest, nipples, arms, wrists, fingers and anogenital region [1]. There have only been three previously reported cases of apocrine adenocarcinoma in the anal/perianal region [2–4]. We report a case of a 72-year-old female with perianal apocrine adenocarcinoma based on pathologic and immunohistochemical evidence.
CASE REPORT
A 72-year-old female with a past medical history of pulmonary embolus on Eliquis and obstructive sleep apnea presented for evaluation of a perianal ‘boil’ with persistent drainage. She had noticed the lesion and symptoms for over a year. There were no pertinent findings in the review of systems. On physical exam, the patient had a 2 cm exophytic, pedunculated nodule that appeared to be a perianal cyst at the 1–2 o'clock position. The patient proceeded to the operating room for excision of the perianal nodule. The nodule was elevated and excised with about a 1-cm margin.
Upon pathologic review, a diagnosis of apocrine adenocarcinoma was made with resection margins negative for tumor in planes of the section. On gross description and sectioning, the specimen had a solid and cystic appearance, with the solid component having a granular tan appearance and the cystic component containing serosanguinous fluid. Histologically, the specimen demonstrated areas of mixed solid and trabecular areas with large nuclei and many prominent mitotic figures as seen in Fig. 1. The specimen stained positive for periodic acid–Schiff–diastase (PAS-D), common epithelial marker cytokeratin 7 and tumor associated antigen gross cystic disease fluid protein 15 (GCDFP 15). The specimen was negative for carcinoembryonic antigen.
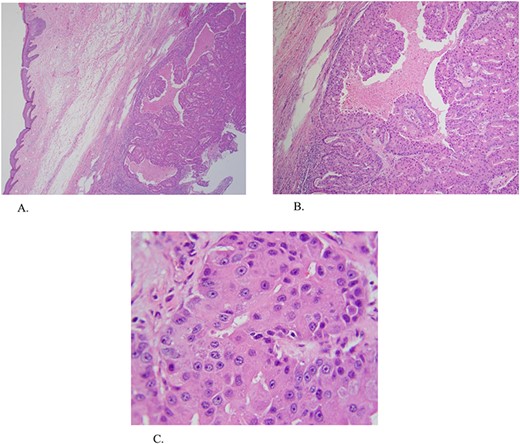
(A and B) ×4 and ×20 magnification hematoxylin and eosin (H&E) stain demonstrating areas of mixed solid and trabecular areas. (C) ×60 magnification H&E stain demonstrating areas with large nuclei and many prominent mitotic figures.
DISCUSSION
Apocrine adenocarcinoma is a rare neoplasm that primarily arises in areas with high apocrine gland density. They have mostly been described in the axilla, but have also been found in regions of the scalp, ear canal, eye lids (Moll’s gland carcinoma), chest, nipples, arms, wrists, fingers and anogenital region. To date, there have only been few case reports describing apocrine adenocarcinoma in the perianal/anal region. We are reporting just the fourth such case.
Apocrine adenocarcinoma is generally a slow growing and indolent tumor [5, 6]. Patients can have highly variable presentation. Most patients are asymptomatic on presentation, but others can experience symptoms of tenderness, purulent discharge or restricted range of motion from the size of the mass [7, 8]. Lesions can be described as erythematous to violaceous, firm, solitary nodules, erythematous patches of skin or ulcerated nodules [2, 6, 8, 9]. As in our patient’s case, she was predominantly asymptomatic until she started experiencing discharge from the area, which brought the pigmented perianal nodular lesion to her attention.
Standard management of apocrine adenocarcinoma has not been established and has been based on consensus from previous reports involving mostly axillary lesions. The literature recommends wide local excision with possible adjuvant options of chemotherapy and radiation [6, 10]. It has been previously reported from reviews of the literature that sentinel lymph node biopsy is recommended because of the high rate (40–50%) of lymph node metastases at presentation based on reports from axillary lesions [6, 9]. Research shows variable results with adjunct chemotherapy and radiation. Adjunct chemotherapy or radiation should be considered in cases with large tumor size, perineural, lymphatic or vascular invasion, or when complete removal of the tumor is not possible due to location or size [6, 10].
Considering apocrine adenocarcinoma has a primarily benign presentation, definitive diagnosis is based on histopathologic features from the surgical specimen. The common histologic characteristics primarily demonstrate apocrine origin with anaplastic features. Tumor cells can be characterized by hyper chromatic nuclei, nuclear pleomorphism, mitotic figures and lack of decapitation secretion [5, 6, 10]. There are various immunohistochemical stains that aid in the diagnosis of apocrine adenocarcinoma. Cytokeratin stains confirm epithelial origin of the tissue, PAS-D is used to identify the mucin stored in intracytoplasmic granules of apocrine cells and the lumen, and GCDFP-15 is associated with apocrine cell origin [7, 10].
Clinically, it is important to keep apocrine adenocarcinoma as part of our differential diagnosis when dealing with lesions in regions with high apocrine gland density. We must have suspicion of such lesions, considering apocrine adenocarcinoma has a benign clinical presentation, yet can have high percentage of lymph invasion on presentation. It is a rare malignancy, yet we should be familiar with the natural history and management options available.
ACKNOWLEDGMENT
The authors would like to acknowledge Joel Horovitz, MD, and Ronald Simon, MD, for the reviewing and editing of this manuscript.



