-
PDF
- Split View
-
Views
-
Cite
Cite
Nobuhito Nitta, Yusuke Yamamoto, Teiichi Sugiura, Yukiyasu Okamura, Takaaki Ito, Ryo Ashida, Katsuhisa Ohgi, Shimpei Otsuka, Keiko Sasaki, Katsuhiko Uesaka, Middle segment-preserving pancreatectomy for multifocal pancreatic ductal adenocarcinoma located in the head and tail of the pancreas: a case report, Journal of Surgical Case Reports, Volume 2020, Issue 10, October 2020, rjaa383, https://doi.org/10.1093/jscr/rjaa383
Close - Share Icon Share
Abstract
A 77-year-old woman with a solitary existence was referred to our hospital for the treatment of pancreatic tumors. Computed tomography revealed an 18-mm mass in the pancreatic head that had invaded the right side of the superior mesenteric vein (SMV) and a 32-mm mass in the pancreatic tail. We performed middle segment-preserving pancreatectomy (MSPP) with SMV resection and reconstruction. The TNM classifications were T2, N1, M0, stage IIB in the pancreatic head, and T2, N0, M0, stage IB in the pancreatic tail, respectively. Postoperatively, the blood glucose was well controlled using only hypoglycemic drug, and insulin preparation was not necessary. No fatty diarrhea was found using a pancreatic enzyme supplement. After 9 months of follow-up, no recurrence was found. MSPP for pancreatic head and tail carcinomas seemed acceptable for both preserving the postoperative quality of life and ensuring curative resection especially in elderly patient with a solitary existence.
INTRODUCTION
Total pancreatectomy (TP) has been selected as the operation for multiple pancreatic lesions; however, metabolic disorders, such as insulin-dependent diabetes mellitus (DM) and severe diarrhea, still remain major problems after TP. Middle segment-preserving pancreatectomy (MSPP) was introduced as an operation that preserves the pancreatic endocrine and exocrine functions [1]. We herein report a patient who successfully underwent MSPP with superior mesenteric vein (SMV) resection and reconstruction for pancreatic head and tail carcinomas.
CASE REPORT
A 77-year-old woman with a solitary existence was referred to our hospital for the treatment of pancreatic tumors. All hematologic examinations including tumor makers were within the normal ranges. Contrast-enhanced abdominal computed tomography revealed an 18-mm mass in the pancreatic head that had invaded the right side of the SMV and a 32-mm mass in the pancreatic tail (Fig. 1a and b). Fluorodeoxyglucose (FDG) positron emission tomography showed the accumulation of FDG in both masses (Fig. 1c and d). No metastatic lesion was found in these images. Endoscopic ultrasound-guided fine-needle aspiration revealed that both masses were adenocarcinoma. Of course, TP was appropriate procedure for these pancreatic carcinomas; however, parenchyma-preserving pancreatectomy was considered due to the patient’s age and postoperative quality of life with a solitary existence. Preoperative computed tomography showed the dorsal pancreatic artery (DPA), which flowed into the pancreatic body (Fig. 2a and b). If it was possible to preserve the DPA and confluence of the splenic vein (SpV), preservation of middle segment pancreas was considered possible.
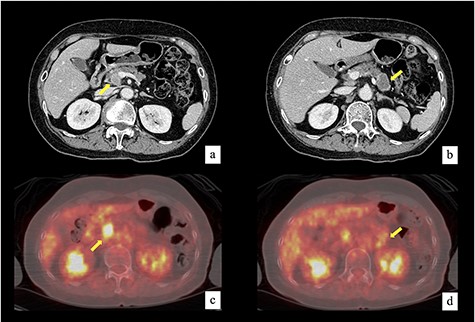
Contrast-enhanced computed tomography revealed an 18-mm mass in the pancreatic head that had invaded the right side of SMV (a) and a 32-mm mass in the pancreatic tail (b). FDG positron emission tomography showed the accumulation of FDG in both masses. The maximum standardized uptake value was 12.9 in the pancreatic head mass (c) and 3.0 in the pancreatic tail mass (d).
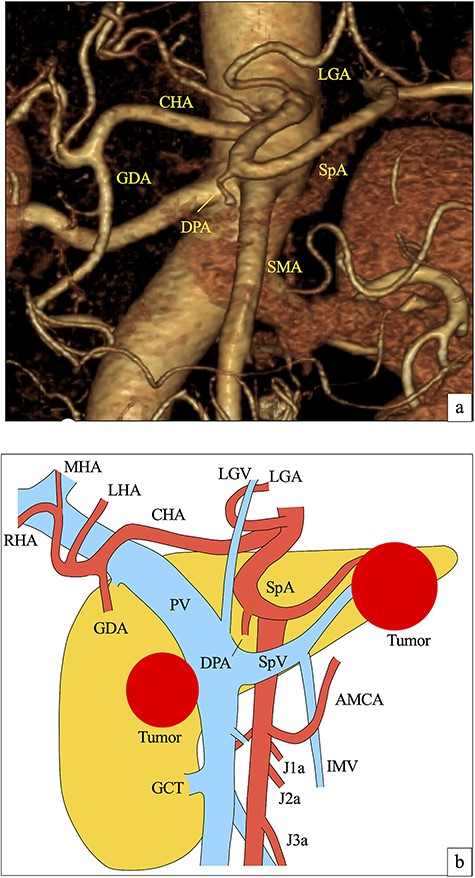
(a) Preoperative 3D computed tomography angiographic image from an anteroposterior view. The DPA branched from the root of the SpA. (b) Preoperative illustration of vessels around pancreas and pancreatic tumors. LGA, left gastric artery; CHA, common hepatic artery; GDA, gastroduodenal artery; LHA, left hepatic artery; MHA, middle hepatic artery; RHA, right hepatic artery; SMA, superior mesenteric artery; AMCA, accessory middle colic artery; J1a, first jejunum artery; J2a, second jejunum artery; J3a, third jejunum artery; LGV, left gastric vein; PV, portal vein; IMV, inferior mesenteric vein; GCT, gastrocolic trunk.
First, we started the pancreaticoduodenectomy procedure. The pancreas was divided at the left side of the SMV. The frozen specimen of the pancreatic stump was negative for cancer. The pancreatic head tumor had invaded the right wall of the SMV (Fig. 3a), suggesting the need for SMV resection and reconstruction. The preservation of the SpV was necessary for MSPP. In order to determine the method of SMV resection and reconstruction about preserving the SpV, we had needed to perform distal pancreatectomy and evaluate the distal pancreatic stump. We then started distal pancreatectomy with splenectomy. The divided line of the distal pancreas was 2 cm on the proximal side of the pancreatic tail tumor. The frozen specimen of the pancreatic tail stump was negative for cancer. The splenic artery (SpA) and SpV were resected at the distal dividing line of the pancreas, preserving the DPA and the proximal side of the SpA and SpV. Lymphadenectomy around the SpA was performed sufficiently. We then decided to perform MSPP. We resected the SMV diagonally from the blood flow of the SMV to preserve the confluence of the SpV, which was necessary as a drainage vein for the remnant pancreatic body (Fig. 3b). After excising the specimen of the pancreatic head, SMV reconstruction was performed by running sutures using 6-0 non-absorbable monofilament (Fig. 3c and d). Finally, 4 cm of the pancreatic body was preserved (Fig. 3e and f). Reconstruction was carried out by a modified Child method. She received long-term drain management for complicated abdominal abscess due to postoperative pancreatic fistula. The blood glucose was controlled well with only dipeptidyl peptidase-4 inhibitor, and insulin preparation was not necessary. No fatty diarrhea occurred using a pancreatic enzyme supplement. The patient was discharged on postoperative Day 96.
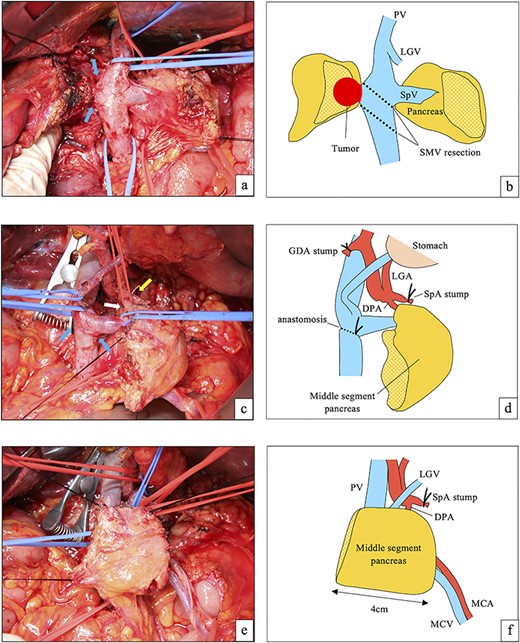
(a) On laparotomy, the pancreatic head tumor had invaded the right wall of the SMV (blue arrows). Distal pancreatectomy was performed. (b) Illustration of (a). The SMV was resected diagonally to preserve the SpV. (c) After reconstruction of the SMV (blue arrows). The SpV was preserved. The white arrow shows the preserved DPA (taped), and yellow arrow shows the stump of the SpA. (d) Illustration of (c). (e) The middle segment of the pancreas was preserved. The length of the remnant pancreas was about 4 cm. (f) Illustration of (e). MCA, middle colic artery; MCV, middle colic vein.
A histopathological examination revealed that both pancreatic tumors in the head and tail were pancreatic ductal adenocarcinoma. The TNM classifications were T2, N1, M0, stage IIB in the pancreatic head and T2, N0, M0, stage IB in the pancreatic tail.
S-1 as adjuvant chemotherapy was administered orally. At 9 months of follow-up, no recurrence was found. The serum albumin level was 4.1 g/dl, and HbA1c was 5.3%.
DISCUSSION
Because of a complete absence of pancreatic endocrine and exocrine functions, patients who undergo TP suffer from insulin-dependent DM and severe diarrhea [2]. Symptomatic hypoglycemia occurs in 79–91% of patients who underwent TP, and 22–40% of patients experienced episodes of loss of consciousness [3–5]. In the current case, the patient was elderly and lived a solitary existence. Regular injection of insulin by herself seemed difficult, and metabolic disorders sometimes induce a critical condition due to abrupt hypoglycemia, which may lead to solitary death. Considering the high rate of loss of consciousness, TP should be avoided in the patients with a solitary existence, if possible. MSPP has the benefits of preserving both the pancreatic endocrine and exocrine functions, and postoperative insulin use was reported to be avoidable in 77% patients who underwent MSPP [6]. Although the use of hypoglycemic drug and pancreatic enzyme supplement were necessary, the deterioration of the quality of life seemed to be minimized after performing MSPP in the present case.
Considering the postoperative pancreatic infraction, the preservation of the vessels of blood supply and drainage for the remnant pancreas is necessary in MSPP [1, 7, 8]. In particular, the preservation of the DPA is essential, as other arteries for the remnant pancreas are divided [7]. In the current case, DPA was preserved, and the pancreatic head adenocarcinoma had invaded the SMV, requiring SMV resection. To preserve the SpV as a drainage vein for the remnant pancreas, we resected the SMV diagonally and reconstructed the SMV (Fig. 3a and b).
Most previous reports on MSPP have described procedures for benign or low-grade malignant lesions, as lymphadenectomy was not necessary [6–8]. In the current case, we reported the first case of one-term MSPP for pancreatic head and tail adenocarcinomas. TP is usually recommended for patients with pancreatic head and tail adenocarcinomas, as MSPP does not allow for complete lymphadenectomy, especially that of the celiac lymph nodes. However, Lee et al. [9] reported that lymphadenectomy of the celiac lymph nodes imbued no survival benefit for pancreatic tail adenocarcinoma. In the current case, lymphadenectomy for the pancreatic tail adenocarcinoma was considered to be adequate, because lymphadenectomy around the SpA was performed sufficiently.
In conclusion, MSPP for pancreatic head and tail carcinomas seems to be a viable option for both preserving the postoperative quality of life and ensuring curative resection, especially in elderly patient with a solitary existence.
ACKNOWLEDGEMENTS
The authors thank all of the people who contributed to this work.
Conflict of interest statement
None declared.
REFERENCES
- computed tomography
- carcinoma
- diarrhea
- follow-up
- hypoglycemic agents
- pancreatectomy
- pancreatic neoplasms
- reconstructive surgical procedures
- blood glucose
- insulin
- quality of life
- pancreatic enzyme
- older adult
- pancreas head
- pancreas tail
- pancreatic ductal adenocarcinoma
- superior mesenteric vein
- transverse spin relaxation time



