-
PDF
- Split View
-
Views
-
Cite
Cite
Osama Haddad, Samuel Jacob, Anthony Pham, Basar Sareyyupoglu, Kenneth Dye, Si Mai Pham, Harvesting left internal thoracic artery via clamshell incision for coronary bypass and lung transplant, Journal of Surgical Case Reports, Volume 2020, Issue 10, October 2020, rjaa363, https://doi.org/10.1093/jscr/rjaa363
Close - Share Icon Share
Abstract
Concomitant lung transplantation and coronary artery bypass grafting operation became more prevalent over the last decade due to the advanced age of recipients. Median sternotomy approach is traditionally used when internal thoracic artery is utilized. Here we report a technique of harvesting the left internal thoracic artery via a clamshell incision for a combined coronary artery bypass and bilateral lung transplant operation in a 71-year-old male with terminal respiratory failure and coronary artery disease.
INTRODUCTION
There is a strong association between pulmonary fibrosis and coronary artery disease (CAD), and the latter is a relative contraindication to lung transplantation [1]. However, coronary revascularization with stents before the transplant or concomitant coronary bypass grafting procedure (CABG) offers a survival benefit to patients who otherwise are denied of lung transplants [2]. Traditionally, CABG with internal thoracic artery conduit is performed via a sternotomy incision. We herein report a case of a bilateral lung transplant with concomitant CABG using the left internal thoracic artery (LITA) that was harvested via clamshell incision, with emphasis on the technical aspects of the procedure.
CASE
A 71-year-old woman with chronic respiratory failure due to hypersensitivity pneumonitis was evaluated for lung transplantation (LTx) and found to have CAD. Coronary angiogram showed a 70% lesion in the left anterior descending artery (LAD) (Fig. 1A); other coronary arteries had mild disease. We did not recommend coronary artery stenting and the associated dual antiplatelet therapy due to the urgency of her condition. Instead, we listed the patient for either a single right or bilateral LTx with CABG to the LAD. Because the donor’s total lung capacity was much smaller than that of the recipient’s we elected to perform a bilateral LTx with CABG. Due to her previous wedge resection in the right lower lobe and elevated right hemidiaphragm, we anticipated dense adhesion in the posterior diaphragmatic area therefore decided to use the clamshell incision for the lung transplant and CABG with the LITA.
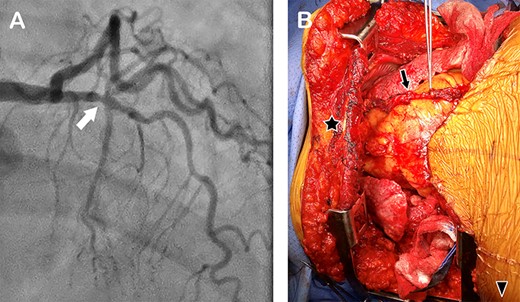
(A) Coronary angiogram showing a stenosis in the left anterior descending artery (arrow); (B) intraoperative photograph of the chest cavity via clamshell incision, showing the harvested LITA lying on the heart (arrow). Star marks the upper sternal edge; arrow head, the patient’s right side.
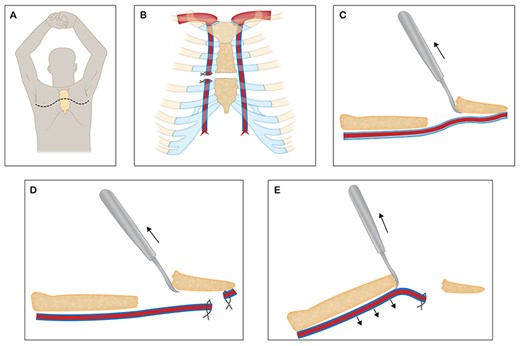
Sketches depicting the harvest of LITA via clamshell incision (A), ligation, division of the RITA and sternum (B), a bone hook was used to lift the lower sternal edge anteriorly and superiorly to expose the distal end of the LITA (C), which was harvested and divided (D), the proximal part of the LITA was harvested by elevating the superior sternal edge with a bone hook (E).
TECHNIQUE
First, right and left anterolateral thoracotomies at the fourth intercostal spaces were performed (Fig. 2A) and the left and right internal thoracic arteries (RITA) were exposed and freed for 2 cm in both directions. We ligated and divided the RITA, then divided the sternum transversely while preserving the LITA (Fig. 2B). Using a bone hook, we lifted the lower edge of the divided sternum superiorly and anteriorly (so as not to put tension on the LITA) to expose the lower part of the LITA (Fig. 2C). We freed the LITA from the chest wall distally and divided it at the bifurcation after administering 3000 units of heparin intravenously (Fig. 3D). By placing two Finochietto retractors in the right and left fourth intercostal spaces, and using a bone hook to elevate the superior edge of the sternum, we were able to expose and harvest the entire upper portion of the LIMA up to its origin (Fig. 2E). The harvested LIMA (Fig. 1A) was covered with papaverine soaked sponge and tucked in the left pleural cavity for later use.
Subsequently the pericardium was opened, heparin (100 units per kilogram of body weight) given to achieve the activated clotting time (ACT) of 180–250 seconds, and standard central aortic and bicaval cannulation were done for venoarterial extracorporeal membrane oxygenator (VA-ECMO). We used bicaval cannulation to avoid inadequate venous drainage when the superior vena cava was retracted to the left side to facilitate exposure for anastomosing the right pulmonary arteries and bronchi. A hybrid ECMO-cardiopulmonary bypass (CPB) circuit that was customized from a regular CBP system is used routinely for lung transplant operation at our institution [3].
With the patient on VA-ECMO, we dissected out both lungs and isolated hilar structures, followed by left pneumonectomy and donor left lung implantation. Subsequently, additional heparin was administered to achieve an ACT level about 500 seconds and VA-ECMO was converted to full CPB. We arrested the heart for the LITA to LAD anastomosis. Subsequently, we transplanted the right donor lung under partial CPB with the heart beating to allow perfusion to the left lung. The patient was weaned off CPB, and the incision was closed after achieving adequate hemostasis. She had an uneventful postoperative course and was discharged from the hospital on postoperative Day 29.
COMMENT
CAD remains a relative contraindication to LTx, however coronary revascularization in selected candidates with discrete lesions may provide survival benefits [4]. The choice of conduit for CABG in lung recipients remains controversial. Given the median survival of 48–60 months after lung transplant [5], saphenous vein grafts (SVG) are reasonable option. However because of the high occlusion rate of SVG (up to 40% in the first 12–18 months) [6], which may be exacerbated by the progression of metabolic syndrome (diabetes, hypertension and dyslipidemia) after transplant, the use of arterial conduit could be justified.
Clamshell incision is a widely accepted approach for bilateral LTx. In comparison to sternotomy, it provides excellent exposure to all thoracic structures including the posterior aspects of the hilum and the diaphragmatic recesses, especially when there are adhesions. It provides easier access to the posterior hilar area for hemostasis and reduces the risk of sternal complications in immunocompromised patients who need tracheostomy.
The utilization of the LIMA also avoided a proximal anastomosis in the ascending aorta and a leg incision if a vein graft was used. To minimize full CPB time and full heparinization duration, we opted to complete lung and hilar dissections, left pneumonectomy and left LTx on VA-ECMO. The coronary anastomosis also can be performed on VA-ECMO with a beating heart if the surgeon prefers. We utilized a combination of VA-ECMO and CPB for the operation because of extremely poor native lung function to allow for ‘off pump’ bypass as described by Khatchatourian et al., on a patient with chronic obstructive lung disease [7]. The technique of the harvesting the LITA with robots through a thoracotomy incision for minimally invasive CABG has been described [8]; however this technique is impractical during lung transplant operation because of the complexity of the setup and the surgical skills required.
In summary, concomitant lung transplant and CABG, especially with LIMA utilization, can be safely done through a clamshell incision and may offer some advantages over a sternotomy incision and saphenous vein conduits.
ACKNOWLEDGMENTS
The institutional review board granted an exception for this case report and waived the consent form.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
References
Kizer JR, Zisman DA, Blumenthal NP,
Castleberry AW, Martin JT, Osho AA,
Thomas M, Martin AK, Allen WL,
Sherman W, Rabkin DG, Ross D,
Christie JD, Edwards LB, Aurora P, Dobbels F, Kirk R, Rahmel AO, et al.
Alexander JH, Hafley G, Harrington RA,



