-
PDF
- Split View
-
Views
-
Cite
Cite
Francisco Lozano, Carola Rubio, Paula Velasco, José R González-Porras, Kinking graft—an exceptional late complication of axillofemoral bypass grafting, Journal of Surgical Case Reports, Volume 2020, Issue 10, October 2020, rjaa324, https://doi.org/10.1093/jscr/rjaa324
Close - Share Icon Share
Abstract
The axillary-femoral bypass is an extra-anatomical arterial reconstruction technique whose indications and complications have been thoroughly discussed in the literature. Shortening or lengthening of the prosthesis (by axillary artery traction or graft angulation, respectively) as a late postoperative complication of the procedure has been described only exceptionally. Here we report a kinking of the prosthesis with a very illustrative figure.
INTRODUCTION
The axillary-femoral bypass, introduced almost 50 years ago by Blaisdell et al. [1], is a well-established and valuable revascularization procedure, used mainly in (i) diffuse aortoiliac occlusive disease in patients with local or systemic contraindications to revascularization by laparotomy, and (ii) ex situ treatment of infected infrarenal aortic prostheses or stents.
CASE REPORT
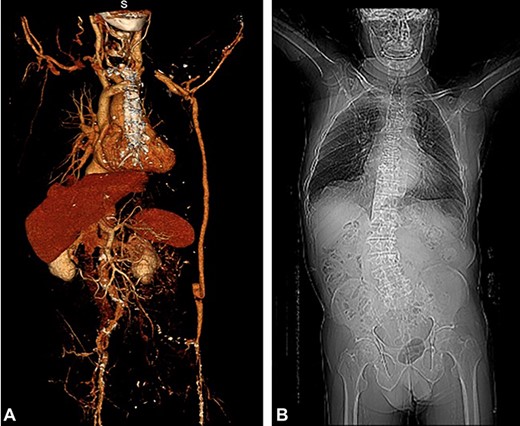
An 85-year-old male, whose background includes: (i) revascularized ischemic heart disease (January 2010), but with subsequent stress angina, and (ii) axillary-femoral bypass (AxF) (July 2018) with a Dacron prosthesis (8 mm in diameter, without external support) due to critical ischemia of the left lower limb secondary to occlusion of the left iliac arterial axis. Twenty-two months after carrying out the AxF, the patient abruptly presented, without prior trauma, with a lump at the level of the abdominal path of the AxF; a mass of 5 cm in diameter could be seen that beats and did not alter the surrounding skin. Patent femoral and popliteal pulses were noted. The patient had an ABI of 0.75. A Doppler ultrasound yielded an image showing a permeable prosthesis and graft angulation. The CT scan confirmed kinking of the prosthesis (Fig. 1). Under general anesthesia, the redundant prosthetic segment was resected and replaced, over a 20-cm section, by a new Dacron-silver prosthesis in the terminal–terminal position. Postoperatively, the patient has so far experienced without no incidents (ABI = 0.80). A microbiological culture taken from the prosthesis was negative. The patient consent to publish their case details and images was obtained.
DISCUSSION
The AxF bypass is an extra-anatomical arterial reconstruction technique whose indications and complications have been thoroughly discussed in the literature [2]. Shortening or lengthening of the prosthesis (by axillary artery traction or graft angulation, respectively) as a late postoperative complication of the procedure has been described only exceptionally [3–4]. These complications are very different from those that appear as a result of technical errors occurring in the immediate postoperative period.
The exact correspondence between the length of the AxF and the size of the patient’s body can change during the postoperative period. On the one hand, excessive weight gain in the patient’s body can make the graft relatively short [3]. On the other hand, multiple fractures of the lumbar vertebrae can lead to a significant shortening of stature [4] or, as in the case of our patient, the development of serious scoliosis (Panel A-2); angulation of the prosthesis facilitates skin ulceration, thrombosis and graft contamination [4].
Although indications and meticulous use of the surgical technique prevent intraoperative and postoperative complications, certain factors, such as those referred to and related to the patient, can lead to complications that cannot always be predicted or avoided.
CONFLICT OF INTEREST STATEMENT
None declared.
AUTHOR CONTRIBUTIONS
FLS was the main author and vascular surgeon; CR and PV were vascular surgeons; JRGP contributed to literature search.
CONSENT
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
ACKNOWLEDGMENTS
We thank theater and vascular surgical staff of the Hospital Universitario de Salamanca for the care of the patient. This work received no external funding.
This study was carried out at Hospital Universitario de Salamanca.



