-
PDF
- Split View
-
Views
-
Cite
Cite
Rabeet Khan, Renu Irri, Effie Katsarma, A rare case of a digital papillary carcinoma of the hand with secondary conservative management, Journal of Surgical Case Reports, Volume 2020, Issue 1, January 2020, rjz403, https://doi.org/10.1093/jscr/rjz403
Close - Share Icon Share
Abstract
A digital papillary carcinoma (DPC) is a cancer of the sweat glands which develops on the digits of the hands and feet. With an incidence of 0.08 per 1 000 000 people/year, it is often initially misdiagnosed as a simple ganglion although it has a significant risk of metastasis. Histological analysis is beneficial in the formal diagnosis of DPCs. In this report, we present a rare case of DPC affecting the palm of the hand, rather than the more commonly reported DPC of the digits. We discuss the management strategy utilized in this case and the various prognostic considerations taken into account when deciding on an amputation versus local excision surgical approach. All cases of DPC require regular follow up imaging for early detection of recurrence or new metastases to maximize prognosis.
INTRODUCTION
A digital papillary carcinoma (DPC) is a rare neoplasm of the sweat glands which predominantly affects the digits of the hands and feet. It was first reported as a benign papillary adenoma by Helwig in 1979 [1] but was later reclassified to an adenocarcinoma in 1987 on the basis of histological findings [2]. More recently, the World Health Organization (WHO) has grouped both terms as a DPC due to the potentially aggressive behaviour of these lesions although the majority tend to behave as low-grade malignant neoplasms [1, 3]. Due to the rarity of these tumours, misdiagnosis may lead to the delay of prompt treatment, increasing the risk of metastasis.
CASE PRESENTATION
We report on a rare case of a potentially malignant DPC affecting the left hand. A 60-year-old male Caucasian gentleman presented with an atypical ganglion like lesion located on the ulnar aspect of the left palm at the level of the fifth metacarpal phalangeal (MCP) joint. The patient initially presented with this lesion in 2014, and a working diagnosis of a palmar ganglion was assumed. Subsequently, aspiration under ultrasound guidance was conducted, as the patient was hesitant to undergo surgical excision. Although there was reduction in size initially, the ganglion recurred and it is gradual increase in size prompted the patient to seek review. On examination, the lesion was mobile with a hard consistency and a diameter of 2.5 × 2cm. There was a good range of movement of the fingers; however, full flexion of the fifth digit was difficult to achieve due to the size of the lesion at the distal palm. Sensation was intact in all fingers in the left hand; however, the capillary time was slightly prolonged. This was supported by a digital Allen’s test, confirming occlusion of the radial digital artery.
MRI findings showed a tri-lobed lesion (Figs 1 and 2) overlying the volar aspect of the base of the proximal phalanx of the left little finger—consistent with a complex ganglion cyst. The lesion was adjacent to but separate from the flexor sheath and the radial neurovascular bundle of the left finger. With malignancy in mind, chest X-ray did not reveal any associated lung lesion or nodularity and an ultrasound scan of the axilla did not elucidate any lymphadenopathy. Consequently, surgical excision of the lesion was performed and histological analysis conducted.
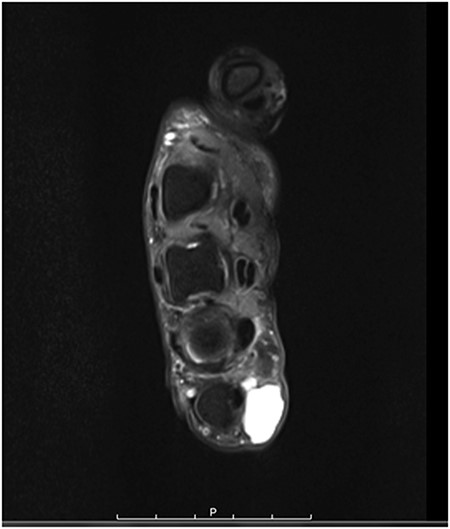
axial MRI scan of the left hand showing the DPC at the level of the fifth MCP joint.
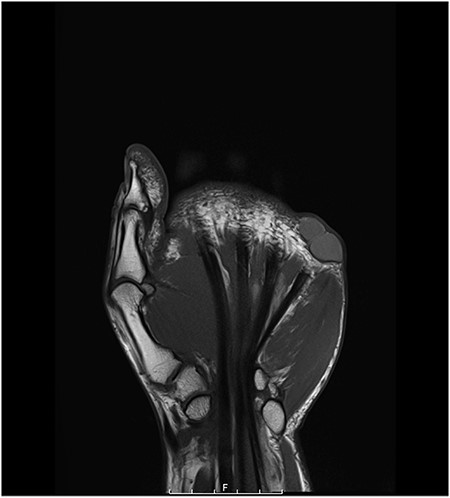
coronal MRI scan of the left hand showing the DPC at the level of the fifth MCP joint.
Excision of the lesion was conducted under general anaesthetic. The specimen was excised in one piece without the excision of surrounding tissue (Fig. 3). Macroscopically, the lesion was well circumscribed, cystic and smooth with a dark brown jelly-like consistency. Histological reporting was challenging and required input from multiple histopathologists for accurate interpretation. The lesion was described as a multiloculated cystic adnexal neoplasm, located within the subcutaneous tissue. There was no evidence of lymphovascular or perineural invasion, but an abundance of mucinous cells was present. The tumour locules were surrounded by a thin border of collagen, indicating likely an adequate resection.
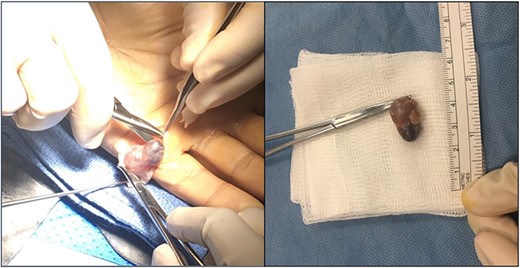
surgically excised DPC. The DPC lesion was excised from the ulnar aspect of the left palm at the level of the fifth MCP joint. The lesion was ~2 cm in diameter and well circumscribed with a dark brown gelatinous appearance.
During multidisciplinary team (MDT) discussion, amputation was considered to be excessive especially if there were to be a completion of excision in the form of scar revision later. Postoperatively, MRI showed scar tissue without any definite residual or recurrence of the lesion. Future management offered to the patient involved scar revision to ensure clear margins after tumour excision and regular follow-up.
DISCUSSION
Previously known as papillary adenomas, papillary carcinomas are rare sweat gland derived neoplasms that predominantly affect the digits of the hands and feet [3]. They are considered to be potentially malignant and have an estimated incidence of ~0.08 per 1 000 000 people/year [4]. Around a 100 cases have been reported in literature previously [5] with the distal digit being a commonly reported location. A DPC tends to present as an asymptomatic non-tender solitary nodule and therefore, patients often wait months to years before seeking medical review [6]. Although the natural progression of DPCs is not well characterized due to the rarity of these tumours, they are known to commonly metastasise to the lung parenchyma [5]. Previous studies noted that these tumours have a 50% local recurrence rate and a 14% metastatic rate [5] with the majority of treatment being either wide local excision or amputation [5, 7]. On histological analysis, DPCs have solid and cystic components and appear as tubuloalveolar ductal structures that can be well circumscribed or infiltrative [3]. Histology can vary between DPCs but the presence of papillary projections is a feature that is always present [8].
Management of this case was challenging due to the rarity of DPCs and the possibility to behave aggressively despite exhibiting benign morphological features [3, 5]. Furthermore, in this case, the DPC affected the distal palm rather than the digits as noted in previous reports [3, 9]. Due to its more proximal location, it was unclear whether this DPC would behave in a similar way to previously reported DPCs or whether it would have an increased risk of metastases. Functionally, the distal palmar location of this lesion negatively impacted the grip strength of the hand. These factors made the decision for wider local excision or amputation of the little finger more complex.
A previous study comparing amputation and excision showed a 66.7 and 57.1% cure rate for patients, respectively, with a 57.1% local recurrence rate in those who underwent local excision [2]. In this case, histological concerns were raised over the risk of future metastases and whether more extensive excision was deemed to be a safer option. However, following MDT discussion and considering the prolonged natural progression of the lesion in this patient, a more conservative management plan was instated. This would provide a compromise between minimizing patient morbidity while also reducing the risk of local recurrence.
CONCLUSION
Achieving adequate resection of locally invasive DPCs is essential in minimizing the risk of recurrence or metastasis. Follow-up imaging of local and distant sites of metastases such as the lungs are required to maximize long-term patient prognosis, yet length and time of follow-up are yet to be standardized.
Conflicts of interest
There are no conflicts of interest to declare.
Funding
This study did not receive any funding.
ACKNOWLEDGEMENTS
No acknowledgements to declare.



