-
PDF
- Split View
-
Views
-
Cite
Cite
Ciaran M Hurley, Daniel Hechtl, Kin Cheung Ng, Jack McHugh, Rishabh Sehgal, Mark C Regan, Biofilm-sealed perforation of the gastric body: a rare sequela of gastric band erosion, Journal of Surgical Case Reports, Volume 2019, Issue 9, September 2019, rjz263, https://doi.org/10.1093/jscr/rjz263
Close - Share Icon Share
Abstract
Laparoscopic Adjustable Gastric Banding is one of the cardinal bariatric interventions and due to its early safety profile, became the mainstay. Major long-term complications of gastric banding include pouch-herniation-dilation and gastric erosion. A 59-year-old female presented to the emergency department with a 2-week history of progressive central abdominal pain and distention on a background history of a laparoscopic adjustable band insertion 11 years previously. Subsequent computed tomography demonstrated an intragastric band erosion. An exploratory laparotomy demonstrated a gastric band eroded through the stomach sealed by a biofilm. Secondary findings included small bowel ischemia and portal vein thrombosis. The gastric band was extracted, and the stomach was repaired. The ischemic small bowel was resected with primary anastomosis. The patient recovered uneventfully. Gastric band erosion should be considered in all patients presenting with abdominal pain and previous weight loss surgery. Prompt recognition may avoid fatal consequences.
INTRODUCTION
Obesity is a worldwide pandemic, which is substantially underestimated in scale and is increasing with exponential growth [1]. Bariatric surgery is able to achieve substantial and durable weight loss and comorbidity reduction for morbid obesity [2]. Level 1 evidence supports the use of bariatric surgery over optimal lifestyle therapies for morbidly obese adults. Gastric banding and gastric bypass techniques are used in >90% of bariatric surgery [2]. Laparoscopic Adjustable Gastric Banding (LAGB) is one of the cardinal bariatric interventions, and due to its early safety profile, became the mainstay. However, more recently, its use has declined due to inconsistent long-term results [3].
Major long-term complications of LAGB include pouch-herniation-dilation and gastric erosion [3]. The diagnosis of gastric erosions, an appropriate surgical management pathway and the expected outcome for the patient are of critical importance. Case report evidence of acute presentations such as unretractable hemorrhage, bowel obstruction and septic complications are described [4]. We describe a rare case of gastric band erosion sealed off by a chronic biofilm filament.
CASE REPORT
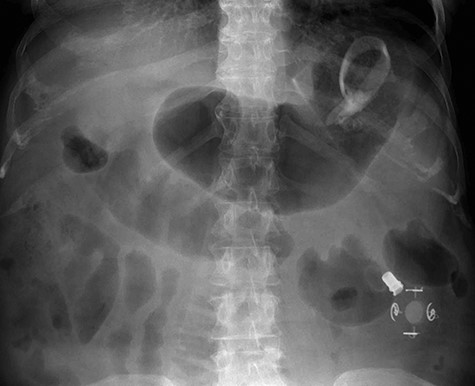
A 59-year-old female presented to the emergency department with a 2-week history of progressive central abdominal pain and distention on a background history of a laparoscopic adjustable band insertion 11 years previously. She had associated nausea, vomiting and denied dysphagia, odynophagia, or change in bowel habit. Clinically, she was afebrile, tachycardic, and on examination, displayed diffuse abdominal tenderness and guarding. Inflammatory markers were mildly elevated (white cell count 13.7 × 109/L, C-reactive protein 105 mg/L), and a moderate hyperlactatemia was observed (lactate 2.4 mmol/L). A plain film abdomen demonstrated a distended, air-filled stomach (Fig. 1). Subsequent computed tomography of the abdomen and pelvis demonstrated an intragastric band erosion with the internalization of the entire gastric band and distal connector tubing within the gastric lumen (Fig. 2). Moderate free fluid and ascites were noted with considerable mesenteric inflammatory fat stranding. The portal vein was non-opacified, indicating a possible portal vein thrombosis (PVT).

The patient was promptly brought to the theater for an exploratory laparotomy. Approximately 30 cm of ischemic small bowel segment with engorged mesentery was identified and resected; while doing so, blood clots were extruding out of the mesenteric vascular arcade. An on-table OGD was performed, demonstrating a deformed shaped stomach. The gastric band had completely eroded through the wall of the stomach. A biofilm had formed around the band device from the distal connecting tubing, tracking into the fundus of the stomach and sealing the perforation (Fig. 3). The biofilm was tracked to the stomach externally, the stomach opened and the device retrieved (Fig. 4). The stomach was closed in two layers and abdominal drains were inserted prior to closure.
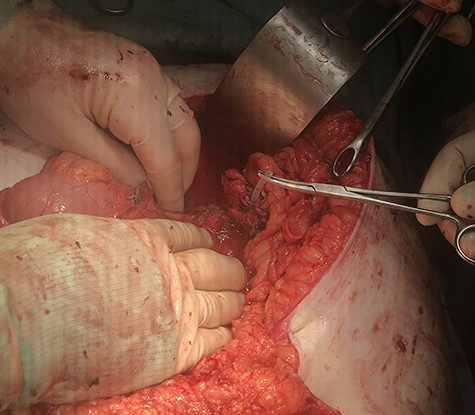
Midline laparotomy demonstrating biofilm-sealed eroded adjustable gastric band.

The patient was monitored in the intensive care unit postoperatively. A focused hepatic ultrasound was performed, which demonstrated an almost completely thrombosed portal vein. The patient was, therefore, commenced on a therapeutic dose of tinzaparin sodium. The patient required intensive gastroenterology, dietician, physiotherapy and hematology input postoperatively. By 3 weeks, prior to discharge, a barium meal demonstrated normal gastric contours with no filling defects (Fig. 5). No gastric outlet emptying was observed.

DISCUSSION
The advent of the laparoscopic adjustable gastric band began with the seminal work of Szinicz and Mueller in Austria, who experimented on adjustable bands in animal models [5]. Banding has since entered into worldwide practice following the emergence of laparoscopic techniques making it possible to insert adjustable bands without open surgery [5]. There have been several iterations in the adjustable band since the 1990s, culminating in the development of the Lap-Band®, which has undergone multiple revisions since its introduction [5].
Current guidelines from the National Institutes of Health recommends consideration for bariatric surgery for patients with a BMI of >40 kg/m2 and for those with a BMI >35 kg/m2 with associated medical comorbidities [6]. The USA favors the Roux-en-Y bypass approach, whereas Europe and Australia predominantly use the LAGB [7]. Despite the absence of randomized controlled trials comparing the outcomes of both, there is abundant evidence to suggest both Roux-en-Y bypass surgery and LAGB accomplish long-term weight loss and durable reduction in morbidity in the obese [5]. In the short term, complication rates favor the use of the LAGB [8]. Operative times are shorter and hospitalization stay is lower [8]. Despite early results, there are concerns that LAGB produces significantly higher reoperation rates in comparison to the Roux-en-Y population [8]. These issues include port problems, band slippage with pouch dilation, gallbladder problems, incisional hernias and gastric band erosion.
Gastric band erosion post LAGB is a recognized complication occurring in ~3% of patients [3, 4, 8]. Risk factors for erosion include a band of 10 cm and the perigastric approach [4]. Typical presentation includes loss of satiety, abdominal pain and port swellings. There is case report evidence of large hemorrhage, bowel obstruction and complications of sepsis [4]. To the authors’ knowledge, there is no report of a gastric band erosion producing a biofilm as described here. The formation of a biofilm indicates the chronicity of the erosion in this case, which leads to drastic patient complications. Most gastric band erosions can be managed with nonurgent revisional surgery occurring months after the onset of symptoms [4]. This presentation of patients was complicated with the presence of a PVT.
PVT is a relatively rare entity linked with the presence of either an underlying liver disease or a prothrombotic disorder [9]. The consequences of PVT are related to the extension of the thrombus [9]. Ischemia may result from extension of the thrombus into the mesenteric veins and venous arches, or from reflex arteriolar vasoconstriction post venous thrombosis [9]. Although there is no report of PVT secondary to LAGB evident in the literature, there is case report evidence of both portal and splenic vein thrombosis as an unusual but severe complication of LAGB infection [10]. In the absence of liver disease, the pathogenesis of this is likely linked to a high inflammatory state and sepsis [9].
In conclusion, we present a rare case of LAGB erosion sealed by a chronic biofilm, which was complicated by PVT and small bowel ischemia. Prompt recognition and management of the clinical context are pertinent to avoid fatal consequences.
ACKNOWLEDGMENTS
The authors have no acknowledgements to any institution or funding body to declare.
References
- ischemia
- abdominal pain
- computed tomography
- anastomosis, surgical
- biofilms
- dilatation, pathologic
- emergency service, hospital
- hernias
- intestine, small
- laparoscopy
- safety
- stomach
- gastric band placement
- portal vein thrombosis
- bariatric surgery
- laparoscopic adjustable gastric banding
- laparotomy, exploratory
- small bowel ischemia
- erosion
- intragastric route



