-
PDF
- Split View
-
Views
-
Cite
Cite
Ali Kordzadeh, Athanasios Syllaios, Spyridon Davakis, Bruno Lorenzi, Naga V Jayanthi, Cheuk-Bong Tang, Alexandros Charalabopoulos, Over-the-scope-clip treatment of gastrobronchial fistula following minimally invasive oesophagectomy: a novel approach, Journal of Surgical Case Reports, Volume 2019, Issue 8, August 2019, rjz229, https://doi.org/10.1093/jscr/rjz229
Close - Share Icon Share
ABSTRACT
Gastrobronchial fistulae (GBF) following minimally invasive oesophagectomy (MIO) is a rare entity, with an estimated incidence of 0.3–1.5% according to the published literature. It could present with persistent cough (Ohno’s sign), chest pain, haemoptysis and recurrent pneumonia. Barium swallow examination remains the most sensitive investigation in 78% of the cases; the main stay of management is surgical and in some cases endoscopic (stent insertion). We report a rare case of a GBF 1 month after two-stage MIO for cancer of the gastro-oesophageal junction, which was successfully treated for the first time with an over-the-scope-clip.
INTRODUCTION
Gastrobronchial fistulae (GBF) following minimally invasive oesophagectomy (MIO) is a rare entity, with a reported incidence of 0.3–1.5% in the published literature [1]. Upon recognition, the mainstay of treatment is open surgery with different types of flaps. Irrespective of the approach, surgical repair has been associated with significant adversity [1]. Herein, we report the first case of GBF successfully treated with an endoscopically placed over-the-scope-clip (OTSC) in an otherwise fit 49-year-old male post-MIO for adenocarcinoma of gastroesophageal junction.
CASE REPORT
A 49-year-old male, with past medical history of tobacco smoking, who was diagnosed with adenocarcinoma of gastroesophageal junction underwent minimally invasive two-stage oesophagectomy. A month following discharge, he presented with complains of chest pain and persistent coughing (Ohno’s sign); barium swallow examination was conducted. This demonstrated a gastrobronchial fistula, between the newly formed gastric conduit and the left main bronchus (Figures 1 and 2). On endoscopic evaluation, a 5 mm communication between the tip of the gastric conduit and the left main bronchus with no evidence of ischemia and well-vascularised edges was noted.
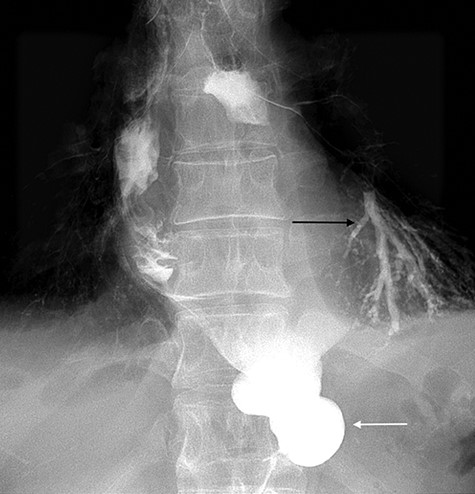
Barium swallow demonstrating the gastric conduit (white arrow) and left bronchial tree (black arrow).
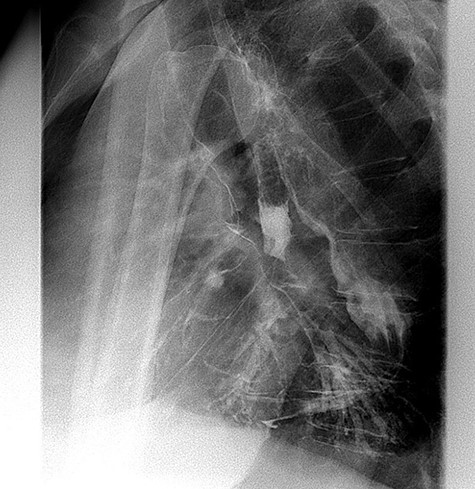
Lateral view of barium swallow demonstrating gastrobronchial fistula.
This was treated with endoscopic OTSC. We approached the GBF endoscopically via gastric conduit. The location of the fistula at the conduit tip made access technically difficult. An endoscopic ‘J manoeuvre’ within the gastric conduit was performed. Upon recognition of the healthy margins within the gastric conduit and of the communicating tract, the application aid anchor was deployed in position. This was followed by alignment of the OTSC and mucosal tissue, with subsequent invagination of the healthy margins within the clip. The fistula required no further intervention.
After this endoscopic procedure, the patient was subjected to barium swallow examination that demonstrated the OTSC on the gastric conduit and no filling of the left bronchus (Figure 3), following by complete resolution of symptoms. At the follow-up time of 6 months, the patient is asymptomatic and there is no recurrence of the fistula. To the best of our knowledge, this is the first reported case of GBF treated with OTSC in the literature.
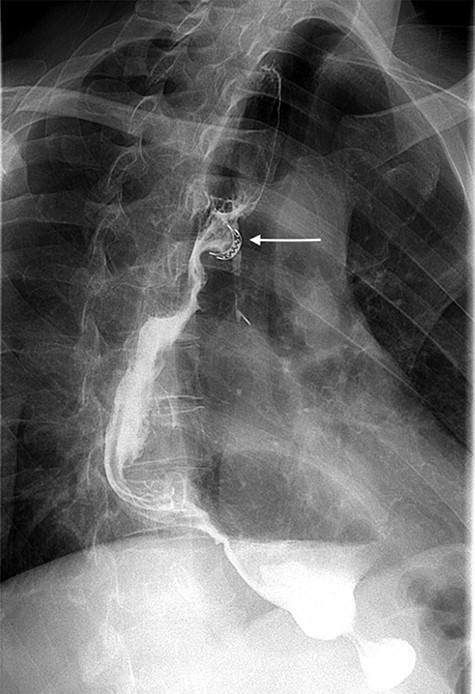
Postoperative barium swallow demonstrating the OTSC on the gastric conduit (white arrow) and no filling of the left bronchus.
DISCUSSION
Stomach remains the first choice and the most favourable conduit substitute following oesophagectomy for operable gastroesophageal junction cancer secondary to its adaptable and hemodynamic nature. However, surgical approach is not free of complications and amongst them, GBF remains a plausible adversity.
In 1985, Moeller and Carpenter [2] classified the aetiology of GBF to five different categories of traumatic injury intraoperatively, redo operations for cancer, ongoing collection or abscess, gastric conduit ulceration and cancer recurrence. However, the time line of GBF presentation varies widely according to the aetiology [2]. The most common cause is gastric conduit ulceration due to unrecognised preoperative peptic ulcer disease or significant stress-induced ulceration (Curling’s ulcer) in the early postoperative course [3].
Nevertheless, intraoperative traumatic injury to the bronchus and/or gastric conduit (ischemia), as well as the presence of an abscess can present early postoperatively, whilst others have a later manifestation. In our case, the most probable cause was a Curling ulcer as no ischemic tissue apart from a 5 mm defect along with inflammation of stomach and intact hand sewn anastomosis was identified.
Patients with GBF can present with a history of recurrent food and liquid expectoration (Ohno’s sign), chest pain, persistent cough, persistent chest infection and haemoptysis [4]. The most sensitive scanning investigation is barium swallow examination, with definite diagnosis in up to 78% of all cases [4]. However, bronchoscopy with pH measurement and contrast-enhanced computed tomography (CT) scan along with upper gastrointestinal tract endoscopy (gastroscopy) can be utilised.
Upon diagnosis, the mainstay of treatment is resection of the fistula and tension-free closure of the gastric conduit and bronchial aperture, with viable and healthy margins. Pectoralis major, intercostal, latissimus dorsi and sternocleidomastoid could be used to interpose the repaired conduit, and in limited circumstances, membranous portion of airway can be substituted with fascia lata, autologous or bovine pericardium [5]. This is achieved via posterior and/or lateral thoracotomy and/or thorocoscopy. This strategy with prolonged hospital stay is associated with significant mortality and morbidity. Furthermore, insertion of a stent in the gastric conduit and airway remains a viable option. In addition, conservative approach in GBF treatment could be trialled; however, to date, only one successful case has been reported [5]. To our knowledge, our case is the first reported case of GBF treated with OTSC in the published literature. Acceptable fistula size for OTSC treatment is a fistoulous opening less than 14 mm (clip’s maximum size closure). Contraindication to this procedure is fibrosis, which may demand debridement of the scar’s tissue before over-the-scope clip’s placement and underlying tumor existence.
CONCLUSION
Small GBF with healthy and viable margins might be amendable to OTSC. In selected cases, this minimally invasive approach could prove beneficial, avoiding a surgical operation and its associated morbidity.
Conflict of interest statement
The authors declare they have no conflict of interest.
Funding
None.



