-
PDF
- Split View
-
Views
-
Cite
Cite
Elias Antoniades, Alkinoos Athanasiou, Panagiotis Sarlis, Ioannis Magras, Ioannis Patsalas, Gross total resection of intracisternal accessory nerve schwannomas using a familiar midline suboccipital subtonsilar approach, Journal of Surgical Case Reports, Volume 2019, Issue 7, July 2019, rjz220, https://doi.org/10.1093/jscr/rjz220
Close - Share Icon Share
Abstract
Intracisternal Accessory Nerve Schwannomas (ANS) constitute a rare clinical entity with only a few cases reported so far. Their symptoms are usually due to brainstem compression and not manifested until they render of great size. Secondary neuropathy and muscle atrophy are other late signs. The hitherto reported literature advocates a suboccipital craniotomy as a suitable approach. In most of the cases the spinal root was the location tumor arose from. Gross total resection was possible to be carried out in most cases with only sporadic tolerable postoperative deficits reported.
We hereby present three cases of patients with intracisternal ANS treated in the same fashion. Two patients were male and one female. Two patients complained of mainly chronic headaches and neck pain, whereas in the third patient the lesion was found incidentally. Only one patient suffered post-operatively cerebrospinal fluid leakage and wound healing complication, which was treated with revision surgery and administration of antibiotics. None of the patients had postoperative neurological deficits. Furthermore, we conducted a review of the relevant literature where we noted that there is no consensus yet with regards to the appropriate surgical approach.
Based on relevant anatomical studies, we advocate that suboccipital subtonsilar approach provides a wide corridor to the area of lesion allowing complete and safe resection of intracisternal ANS. We thus support that, in most cases, the neurosurgeon should consider using this familiar approach for treating this rare lesion.
INTRODUCTION
Accessory nerve’s Schwannomas (ANS) constitute a rare clinical entity that is often classified with the schwannomas of the other lower cranial nerves. Julow et al. [1] categorized ANS as either intraforaminal or intracisternal. Due to their rarity, an optimal operational approach for purely intracisternal ANS has not yet been standardized. Nonetheless, the hitherto reported cases demonstrate that a midline suboccipital approach with combined laminectomy of the first cervical vertebra (C1 laminectomy) is sufficient for achieving gross total resection and presents itself as the gold standard [1]. We hereby present three cases that were treated similarly and further strengthen this observation.
CASES REPORT
The first of our patients was a 43 years-old man who presented with a space-occupying lesion (SOL) in the cisterna magna adjacent to foramen magnum (FM). His main complaints were neck pain and headache accompanied by dizziness and tinnitus. His magnetic resonance imaging (MRI) revealed a well-circumscribed tumor abutting FM demonstrating high intensity on T1-post contrast sequences and measuring 1.6 × 2.1 cm (Fig. 1a and b). The patient underwent a midline suboccipital craniectomy and C1 laminectomy. Neurophysiologic monitoring was carried out but uneventful. A wound revision followed, due to postoperative complication by cerebrospinal fluid (CSF) leakage and meningitis, requiring prolonged hospitalization for antibiotics administration. Postoperative MRI revealed no tumor residuum (Fig. 1c). The patient was discharged relieved of pain and without new neurological deficit.
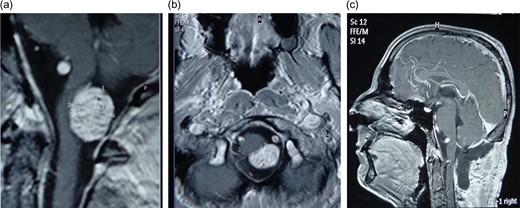
(a) MRI scan of first patient-Accesory nerve neurinoma sagittal plan (b) axial plane showing medulla attachment (c) postoperative MRI scan showing total tumor resection.
The second patient was a 36 years-old woman with medical history of chronic renal failure and secondary hypoparathyroidism. She had to undergo an MRI-scan of brain and cervical region to exclude ectopic parathyroid function. Her examination revealed incidentally a SOL that was high intensity on T1-sequences with dimensions of 1.1 × 1 cm at the level of the FM (Fig. 2a). She reported intermittent numbness of her upper extremities for the two last months. Again, gross total tumor resection was performed via a midline suboccipital craniectomy and C1 laminectomy (Fig. 2b). Intraoperative neurophysiologic monitoring was uneventful. The patient presented no postoperative complications and was discharged neurologically intact.
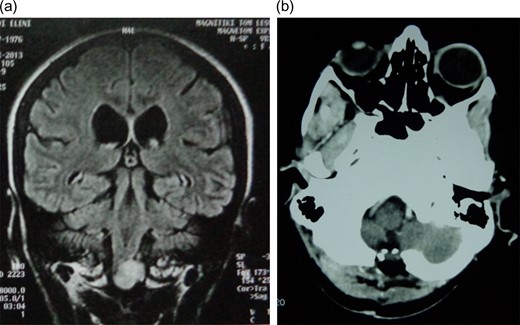
a) Coronal plane of preoperative MRI scan depicting a highly intense of foramen magnum of second patient. (b) Postoperative computer tomography (CT) scan showing total tumor resection.
Our third patient was a 45-year-old man who complained of headaches and neck pain. After a head-MRI was obtained he was diagnosed with a T1-hyperintense 1.2 × 1.3 cm SOL at the right FM, with a central hypointense signal interpreted as intratumoral necrosis. Resection followed via a midline suboccipital approach with C1 laminectomy under uneventful neurophysiologic control. Postoperatively pain receded completely and the patient was discharged home clinically unimpaired.
DISCUSSION
Intracisternal ANS constitute a subcategory of jugular foramen schwannomas. They do not manifest with clinical symptoms until reaching great size, then often presenting with cerebellar signs or myelopathy [2].
Due to increased risk for morbidity total resection is not always attempted and several recent reports advocate a programmed subtotal excision followed by stereotactic radiosurgery of residual tumor so as to minimize postoperative cranial neuropathies. Criteria for choosing a subtotal near total resection may include either attachment to the abducens or facial nerves, adhesions to anterior and posterior inferior cerebellar arteries (PICA) or to any other lower cranial nerves and patient’s age of over 60 years [3]. On the other hand, Kaye et al. [4] first proposed a distinct classification system and recommended a suboccipital craniotomy for tumors presenting minimal extension to jugular foramen, postoperatively demonstrating no new permanent neurological deficits.
Moreover, recent literature also advocated a retrosigmoid approach. Bulsara et al. [1] reviewed a number of previous classification systems and established a modified version referring high extirpation rates for exclusively intracranial tumors. Nonetheless, it is noteworthy that a retrosigmoid approach to structures below the foramina of Luschkas and adjacent to the cerebellomedullary fissure is limited by the flocculus and the plexus choroideus [5]. Alternatively, transcondylare approaches with their variations provide access to lower cranial nerves via the premedullary cistern [5] demanding, however, longer surgical times and are associated with long-term instability of the occipito- cervical junction [5].
Based on our experience and after reviewing the literature [2] the classical midline suboccipital subtonsilar approach can provide full view of the intracisternal segment of lower cranial nerves [5]. Furthermore, it is safer procedure than more complicated combined or non-combined approaches and provides access to the cerebellomedullary cistern, exposing with minimal retraction the jugular foramen and its pathologies [5], being able to also expose more distal segments of posterior inferior cerebellar artery (PICA) and proximal vertebral artery.
CONCLUSIONS
Intracisternal ANS constitute a rare clinical entity. Due to, so far, limited literature there is yet not a clear consensus regarding optimum surgical treatment. Gross total resection remains nonetheless a suitable procedure. Their presence in cerebellomedulary cistern renders them accessible with midline suboccipital subtonsilar approach, offering security and efficacy. The sporadic so far references corroborate our observations.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- antibiotics
- accessory nerve
- craniotomy
- muscular atrophy
- neck pain
- neurilemmoma
- repeat surgery
- spinal nerve root
- surgical procedures, operative
- wound healing
- neoplasms
- neurosurgery specialty
- neuropathy
- posterior fossa compression syndrome
- cerebrospinal fluid leak
- headache, chronic
- neurologic deficits
- consensus



