-
PDF
- Split View
-
Views
-
Cite
Cite
Desiree Dorleijn, Arthur van Noort, Guus Janus, Short-term results of total shoulder arthroplasty for ochronotic arthritis, Journal of Surgical Case Reports, Volume 2019, Issue 7, July 2019, rjz219, https://doi.org/10.1093/jscr/rjz219
Close - Share Icon Share
Abstract
Alkaptonuria is a rare inherited autosomal recessive disorder resulting in large joint osteoarthritis with black discoloration of the cartilage. The glenohumeral is the third most affected joint. Two cases of ochronotic shoulder arthropathy with three shoulder joint replacements are presented. Stemless shoulder arthroplasty was implanted with moderate to good results up to 2 years follow-up regarding pain and range of motion.
INTRODUCTION
Alkaptonuria is a rare inherited autosomal recessive disorder caused by a deficiency of homogentisic acid-oxydase enzyme [1, 2]. Prevalence ranges from 1:200,000 to 1:1000,000 [2, 3]. Homogentisic acid is excreted in urine and changes to dark when exposed to air because of oxidation [2].
The deficiency of the enzyme results in deposition of homogentisic acid pigment in connective tissues, also called ochronosis [4]. Ochrontic pigment deposition in joints results in black discoloration of the cartilage [1, 5]. Large joint osteoarthritis (hip, knee and shoulder) develops after the third decade; peak incidence of ochronotic arthropathy is the fifth decade [1, 3]. The knee joint is affected most, followed by hip and shoulder. The small joints of hand and foot usually are not affected [3, 5].
There is no specific medical treatment that cures the disease [1, 5]. Currently, treatment consists of a protein-restricted diet, with restriction of foods containing phenylalanine and tyrosine. This reduces the production of homogentisic acid and thus limiting symptoms [3]. Treatment of ochronotic osteoarthritis is symptomatic with joint replacement in end-stage osteoarthritis [2].
Literature on joint replacement in ochronotic osteoarthritis is scares and reports mainly case reports on joint arthroplasty for hip and knee [5]. This article presents two cases of shoulder joint replacement for severe ochronotic shoulder osteoarthritis.
CASE REPORT
The first case is a 50-year-old man who works as a butcher. He has alkaptonuria, which was confirmed in a biopsy taken at a knee arthroscopy in 2010. He reports pain in his left shoulder. Physical examination shows an active and passively restricted range of motion. Radiological examination (Figure 1) shows glenohumeral osteoarthritis of the left shoulder. MRI shows an intact rotator cuff with signs of tendinopathy. A stemless cementless total shoulder arthroplasty was implanted (Shoulder Modular Replacement (SMR) Stemless, LIMA) (Figure 2). During surgery, the rotator cuff was intact. One year after implantation patient was satisfied regarding pain and functioning, radiography did not show any signs of loosening or other complications.
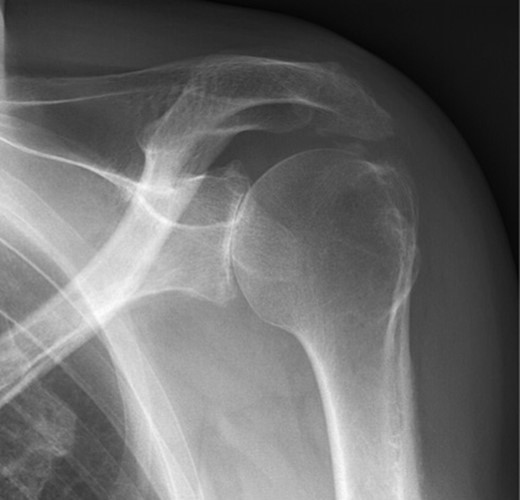
X-ray of left shoulder of patient with ochronosis. AP external rotation view showing glenohumeral osteoarthritis.
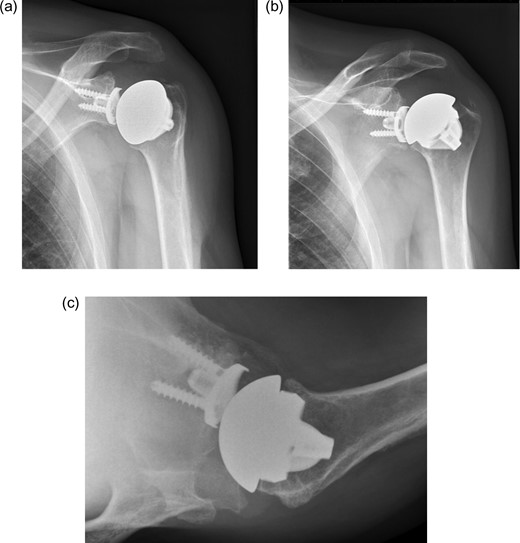
X-ray of left shoulder with total shoulder arthroplasty one year post-operative. (a) AP external rotation view. (b) AP internal rotation view. (c) Axial view.
The second case is a 43-year-old female. She has alkaptonuria and chronic pain in both shoulders. Range of motion is limited in all directions. Radiologic examination shows osteoarthritis of both shoulders. MRI of the shoulder showed good condition of the cuff. A stemless total shoulder arthroplasty was performed on the left side. Peri-operative the humeral head showed obvious signs of alkaptonuria and an intact rotator cuff. (Fig. 3) One year later, a stemless cementless total shoulder arthroplasty was placed on the right side. At follow-up 2-year after left shoulder arthroplasty and 1-year after right shoulder arthroplasty patient was pain free, satisfied, and had a moderate active range of motion of both shoulders (Fig. 4). Active range of motion shows an anteflexion of 80, and an abduction of 70 on the left hand side and anteflexion of 80, and abduction of 60 on the right-hand side. Radiologic follow-up showed no signs of loosening.

Humeral head of patient with ochronosis showing blackish discoloration of cartilage.
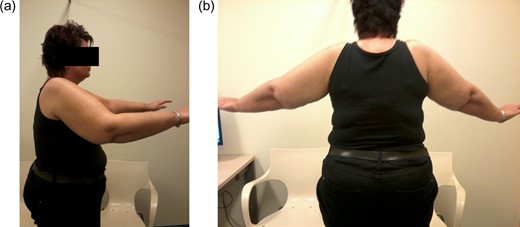
Range of motion of patient with bilateral total shoulder arthroplasty. a) Anteflexion. b) Abduction.
DISCUSSION
Patients with ochronotic arthropathy are relatively young (average 55 years) at joint replacement [3]. Literature on joint replacement is limited to case reports and case series with short to mid-term follow-up of knee replacement and hip replacement [2, 3, 5]. These case series show good results of joint replacement.
The shoulder joint is the third most affected joint in ochronotic arthropathy, but there are few reports on treatment of shoulder ochronotic arthropathy [1, 5].
Gupta et al. present a case of ochronotic shoulder arthropathy that improved in pain and function after arthroscopy and debridement of hypertrophied synovial tissue [1]. Peroperative brown-black discoloration of synovium was seen, as well as erosion of glenoid, labrum, and humeral head. Biopsy was performed and histopathology showed nonspecific inflammation with brown-black pigmentation. Diagnosis of alkaptonuria was confirmed with urine examination. One year after arthroscopy the patient was able to perform daily activities with little pain [1]. Therefore, Gupta et al. conclude that arthroscopy is a therapeutic tool in patients with ochronotic shoulder arthropathy to improve symptoms and range of motion.
Shoulder arthroplasty for patients with ochronotic shoulder arthropathy has been described by Spencer et al. [5] They report on a 60-year old woman with ochronotic shoulder arthropathy in which a shoulder hemi-arthroplasty was performed. The patient was asymptomatic with restricted range of motion at 8 years follow-up. There were no signs of loosening on radiography. Spencer does not report on possible osteoarthritis signs of the glenoid.
We present two patients with ochronotic shoulder arthropathy treated with three shoulder arthroplasty showing good short-term results.
A stemless (‘canal-sparing’) shoulder arthroplasty was chosen because it provides ease of revision, limited bone loss, and optimal restoration of anatomy. A stemless shoulder arthroplasty has a lower risk of peri-operative fractures compared to stemmed arthroplasty. Relative contra-indications for stemless shoulder arthroplasty are different types of metabolic bone disease and/ or poor bone structure. Although alkaptonuria is a metabolic disease, it does not affect bone structure.
Stemless shoulder arthroplasty has been available since 2004 (TESS, Biomet Zimmer) [6]. Today, seven different stemless humeral implants are available, one of which is FDA-approved (Simpliciti Stemless, Tornier). A recent systematic review on 929 cases of stemless anatomic shoulder arthroplasty reports promising clinical and radiological outcomes in short to mid-term follow-up (up to 72 months) [7]. However, in most cases primary osteoarthritis was the indication for shoulder arthroplasty, there were no cases with ochronotic arthropathy.
A SMR Stemless arthroplasty of Lima was implanted in our patients, which is available since 2015.
Literature reports on this arthroplasty are limited, since it is a relatively new arthroplasty. Our own unpublished data (AN) of a ongoing trial show complete satisfaction in 17/18 patients with a SMR stemless arthroplasty with a minimum of 1 year follow-up.
To conclude, in ochronotic shoulder arthropathy a stemless shoulder arthroplasty shows good results in short-term. Longer follow-up is needed to evaluate mid-term follow-up in this specific patient group.
CONFLICT OF INTEREST STATEMENT
None declared.



