-
PDF
- Split View
-
Views
-
Cite
Cite
Stefan Tserovski, Simona Georgieva, Radoil Simeonov, Amir Bigdeli, Heinz Röttinger, Plamen Kinov, Advantages and disadvantages of 3D printing for pre-operative planning of revision hip surgery, Journal of Surgical Case Reports, Volume 2019, Issue 7, July 2019, rjz214, https://doi.org/10.1093/jscr/rjz214
Close - Share Icon Share
Abstract
Total hip arthroplasty (THA) is one of the most successful and cost-effective interventions in medicine nowadays, providing reliable pain relief and functional improvement to those with osteoarthritis or inflammatory arthritis of the hip (P Kinov, B Antonov,’Possibilities for surgical treatment of acetabular osteolysis subsequent to revision arthroplasty of hip joint‘, Orthop Trauma. 52, 2015). Revision hip arthroplasty or severe reconstructive procedures in cases with significant anatomical defects require skilled surgical staff and accurate preoperative planning, including bone insufficiency, deficiency, discontinuity (anatomical assessment) as well as augmentation, cage or other requirements. (implant planning). Some authors recommend preoperative 3D model planning for precise anatomical assessment and preoperative training. This method has some limitations but could be successfully used in addition to conventional surgery.
INTRODUCTION
3D printing was initially introduced by Charles Hull in the 1980 s. The technique was described as ‘stereolithography’ [1]. This technique allows the transformation of a CAD file into a.stl-filethat can be later uploaded onto a 3D printing machine [2]. The uploaded data includes shape, texture and thickness of the object to be printed. The first commercially available 3D printer was introduced by Hull in 1988 and later developed by many other companies.
The manufacturing industry has been using 3D printers ever since they were developed mainly to create models and molds. For that purpose, fast 3D printers called ‘rapid prototyping machines’ are used [1]. 3D printing is currently a $700 million industry with over $110 million invested in medical application [1].
Medical application of 3D printers for production of custom-made medical products: customized prosthetics, patient-specific implant manufacturing—hip and knee joints, precontoured plates, prosthetic implants for ear ossicles, dermal skin grafts, cranial prothesis, scaffolds as vertebral cages as well as menisci, patient-specific antibiotic impregnated articular cement spacers, patient-specific instrumentation to improve the precision and clinical outcome of surgical procedures, anatomical models and simulation tools.
3D printed models represent a new concept for preoperative planning with real scale probe testing of a specific implant [3]
CASE PRESENTATION
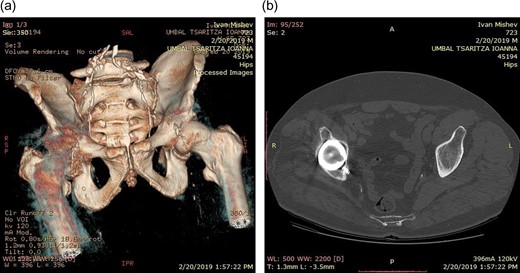
Life-size 3D model was printed from a converted file containing the computed tomography (CT) scan of one patient with severe acetabular defects waiting for total hip revision surgery. The 66-year-old male had a background of coxarthrosis. He underwent total hip arthroplasty of his right hip in February 2017. The preoperative CT scan and X-Ray of the pelvis showed large right-sided pelvic defect and severe acetabular defect (Figs 1 and 2). The patient had history of cardio-vascular comorbidity and underwent 2 week specific antihypertensive therapy preoperatively.

Preoperative radiograph demonstrating large acetabular defect with screw penetration.
We started with rapid prototyping: high resolution protocol with a slice thickness of 1 mm was used to achieve maximal image quality. The CT scan was converted and imported to 3D Slicer, imaging processing software (IPS). Using the IPS we treshholded the image, achieving differentiation of the pelvis and hip from the surrounding soft tissue. We digitally segmented the pelvis by deleting pixels, representing additional bony contact. The right side of the pelvis was isolated. The segment of interest was saved in.stl-format (stereolithographic format), suitable for the 3D printer we used, in our case a Formlabs 2. The.stl-format allows instructions related to the shape, thickness, and texture of the 3D image to be communicated to the 3D printer [3]. Our patient needed 3D planning of the acetabular reconstruction only, as the femur had normal shape. The 3D model enabled visual assessment of the complex acetabular deformity. Given the complexity of our case, the hemipelvis model allowed a life-size anatomical representation of the operative field. (Fig. 3)
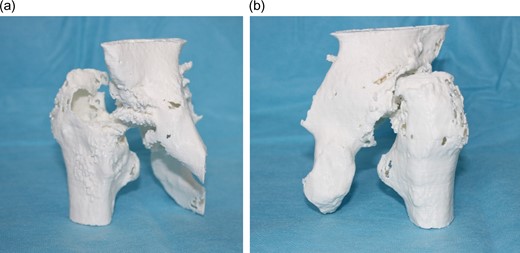
a) Life-size 3D model (anterior vi6ew). (b) Life-size 3 model (posterior view).
We discussed all possible surgical tactics [4]. We could easily recognize all areas of bony deficiency. The model allowed preoperative surgical drill with position simulation (Figs 4–7).

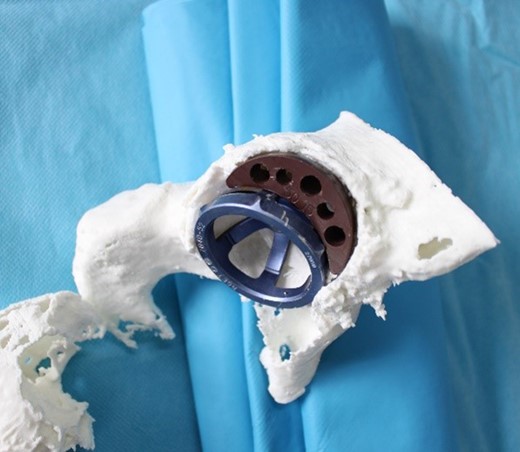
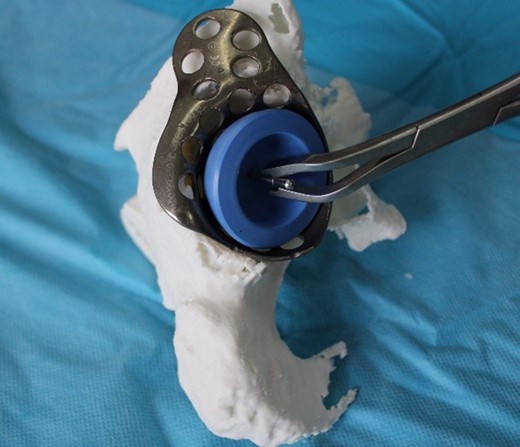
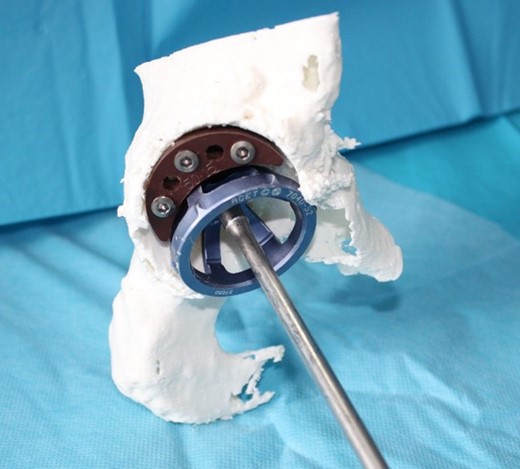
The correct acetabular cup and augment were selected. Preoperative implantation on the 3D model of pressfit cup with augment (Fig. 7).
The surgery was uneventful and a trabecular metal cup with semilunar augment were implanted (Zimmer, Warsaw, IN). The femur was reconstructed with a cementless Alloclassic stem (Fig. 8)

Clinical outcome in the early postoperative period was satisfactory. Standard postoperative rehabilitation protocol was applied with early walking on the first postoperative day and partial weightbearing for 6 weeks. Antibiotic prophylaxis and low molecular weight heparin were administered.
DISCUSSION
The present case illustrates the implementation of preoperative evaluation based on a 3D model.The internal structure is represented as a life-size 3D structure that can be held, rotated, and viewed by the orthopedic team prior to the upcoming procedure [5]. 3D model acetabular assessment was performed by Hurson et al. in 20 patients. In two of the cases the initial surgical approach was altered after further review of the 3D printed acetabular models [6]. Our model improved diagnostic accuracy and helped us predetermine the implant and the implant size. Complex acetabular deformity reconstruction was planned and managed efficiently with good surgical outcome. The accuracy of the model enabled safe preoperative planning and exact reconstruction of the joint [7, 8]. Won et al. demonstrated that this technique can reduce intraoperative complications [9]. Performing 3D printed preoperative planning could reduce anesthetic exposure. The life-size model planning could be used for teaching (residents, students, young specialists). The 3D models provide a field for anatomical teaching for complex pathology in a simulated situation without any risk [10].
The 3D-printing process demonstrates some negative features: it is a technically demanding process, which requires advanced computer skills and additional training. It is also a time extended process, as the completion of each model usually takes about 12 hours. In one of our cases we experienced a technical failure of the model during printing, which extended this timeframe even further. The 3D template is accompanied by a CT- scan of every patient, which makes it more expensive and therefore requires additional radiation exposure as compared to conventional surgery.
REFERENCES
- arthritis
- cost effectiveness
- hip region
- hip joint
- laparotomy
- osteoarthritis
- osteolysis
- pain
- preoperative care
- surgical procedures, operative
- wounds and injuries
- hip replacement arthroplasty
- arthritis, inflammatory
- operative procedure on hip
- hip arthroplasty revision
- implants
- printing, three-dimensional



