-
PDF
- Split View
-
Views
-
Cite
Cite
Mohsin Khan, Aloy J Mukherjee, Hiatal hernia and morbid obesity—‘Roux-en-Y gastric bypass’ the one step solution, Journal of Surgical Case Reports, Volume 2019, Issue 6, June 2019, rjz189, https://doi.org/10.1093/jscr/rjz189
Close - Share Icon Share
Abstract
Obesity and hiatal hernia go hand in hand as siblings. Morbidly obese patients commonly have gastroesophageal reflux (GERD) and associated hiatal hernias (HH). The gold standard for all symptomatic reflux patients is still surgical correction of the paraesophageal hernia, hiatal closure and fundoplication. Laparoscopic Roux-en-Y gastric bypass (LRYGB) is an effective surgical treatment for morbid obesity and is known to effectively control symptoms of gastroesophageal reflux (GERD). It appears to be safe and feasible and becoming more common. Moreover, LRYGB plus Hiatus hernia repair (HHR) appears to be a good alternative for HH patients suffering from morbid obesity as well than antireflux surgery alone because of the additional benefit of significant weight loss and improvement of obesity related co-morbidity. One patient suffering from giant hiatal hernia and morbid obesity where a combined LRYGB and HHR without mesh was performed is presented in this paper.
INTRODUCTION
Obesity is a significant independent risk factor for gastroesophageal reflux disease (GERD) and hiatal hernia (HH). The incidence of HH increases with body mass index (BMI). Hiatal hernia repair (HHR) and fundoplication is the standard surgical treatment for HH. However, much higher recurrence rates are observed in morbid obese patients with BMI levels over 35 kg/m2. Laparoscopic Roux-en-Y gastric bypass (LRYGB) is one of the most performed surgical treatment for morbid obesity and also controls symptoms and complications of GERD. Only few cases are reported of morbidly obese patients with paraesophageal hernias in which LRYGB was combined with primary crurae closure [1, 2]. These procedures appeared to be feasible and safe. Combining HHR with a LRYGB procedure may be a better option for morbidly obese patients suffering from giant hiatal hernias than HHR and fundoplication. Here, we report a patient with a giant HH where LRYGB with HHR was performed.
CASE
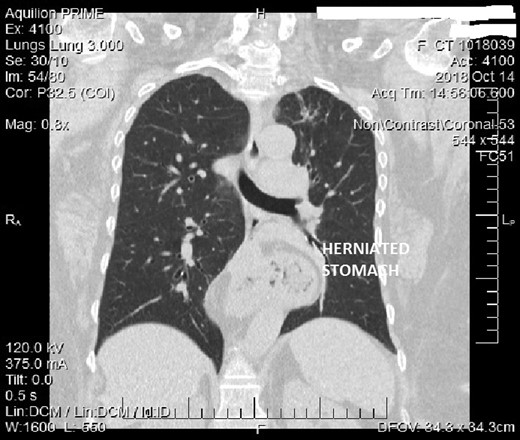
A 63-year-old woman with a height of 161 cm and weight of 116 kg (BMI 44.8 kg/m2) presented with progressive dyspnea, mostly present when bending over, coughing, belching, regurgitation and pyrosis. Medical history revealed hysterectomy 30 years back and hypertension since 10 years. Besides her morbid obesity, there were no other findings revealed by physical examination. CT scan revealed a mixed sliding and paraesophageal hernia, with almost half stomach in the chest (type 4 hiatal hernia) with cholilithiasis (Fig. 1). All relevant investigations, PAC and physician clearance was done. Benefits and risk factor of the surgery were explained and consent for laparoscopic / open haital hernia repair with cholecystectomy with RNYGB taken.
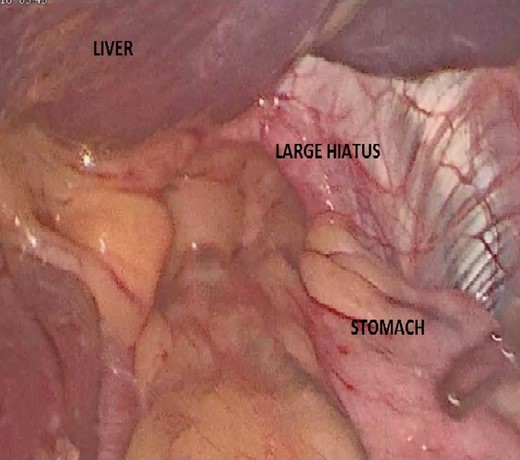
A surgical intervention combining a LRYGB with HHR and cholecystectomy was performed. Large hiatus/diaphragmatic hernia with almost half of stomach into the mediastenum with adhesions around was found (Fig. 2)-Adhesiolysis done and stomach pulled out from defect. Hiatus hernia repair was done with Ethibond 2'0 approximating crural fibers and rosseti plication stitch at angle of his was taken. RNYGB done with—BP limb 50 cm anastomesd to alimentory limb at 150 cm -jejunojejunostomy. Gastric pouch of 50 ml created using blue and purple catridge Gastro Jejunostomy done using ORIVL endo GI stapler 25 mm (anticolic antigastric isoperistaltic GJ). Mesenteric and peterson’s defects were closed. Oral gasrograffin study on day 1showed free passage of contrast into jejunum.patient was ambulated in 2 hours postoperatively and allowed oral liquids after gastrograffin study and subsequently discharged on fourth postop day.
There were no intraop/postoperative complications.
DISCUSSION
Both GERD and HH are highly prevalent among the morbidly obese population with prevalence rates ranging from 39–61% for GERD [3] and 20–53% for HH, respectively. Increased intra-abdominal pressure as a result of central obesity predisposes obese patients for both GERD and HH.
Morbid obese patients that want bariatric surgery are most frequently treated with LRYGB if they are also suffering from GERD, because it results in a reduction of the gastric content, prevention of bile reflux to the gastric pouch and a decrease of intra-abdominal pressure due to the weight loss. As a consequence LRYGB results in a very good control of GERD [4]. But contrariwise not many patients presenting with GERD symptoms who also have morbid obesity are offered this option. The gold standard for all symptomatic reflux patients with morbid obesity is yet to be established. Therefore, it makes sense to combine HHR with bariatric surgery, preferably LRYGB, since this is considered the gold standard for bariatric surgery] and has proven to be effective in controlling GERD in obese patients [4].
In our patient, we decided not to use a mesh to reinforce the sutured crurae as we believed weight loss induced by the LRYGB would lower the abdominal pressure and therefore the chance of HH recurrence. Furthermore, using a mesh in potentially infected areas such as the gastrojejunal anastomosis might cause infection of the mesh as well as erosion of a mesh in the GI-anastomosis.Although biologic meshes as an alternative may not result in more complications and might be considered to reinforce the sutured crural defect.
In our patient, we observed a very smooth post-operative course with significant improvement in pyrosis and weight loss. Taking this in consideration, we would advocate that combined LRYGB and HHR should be considered as the first treatment of choice in patients with a symptomatic paraesophageal hernia and morbid obesity
Few case reports show that concomitant primary crus closure of the HH and LRYGB is feasible and safe [1, 2] and their results are in accordance with ours reporting a EWL of 30% at a follow-up of 6 months [1] and a mean EWL of 46.1% at a follow-up of 12 months [2] and a 100% improvement in GERD symptoms in all cases. In addition, Kothari et al. [5] showed no increase in morbidity and mortality after LRYGB with HHR compared to LRYGB alone. To conclude,for Hiatal hernia and Morbid obesity- ‘Roux-en-Y gastric bypass’ seems to be the one step ideal solution which is safe and feasible
CONFLICT OF INTEREST STATEMENT
None declared.



