-
PDF
- Split View
-
Views
-
Cite
Cite
Keisuke Kamada, Hiroto Kitahara, Yuta Koichi, Naohiro Wakabayashi, Hayato Ise, Chiharu Tanaka, Sentaro Nakanishi, Natsuya Ishikawa, Hiroyuki Kamiya, Delayed thoracic wall bleeding after minimally invasive mitral valve repair, Journal of Surgical Case Reports, Volume 2019, Issue 6, June 2019, rjz187, https://doi.org/10.1093/jscr/rjz187
Close - Share Icon Share
Abstract
The first case of late thoracic wall bleeding after minimally invasive mitral valve repair treated by endovascular therapy is reported. A 55-year-old woman underwent mitral valve repair and tricuspid annuloplasty through a mini-thoracotomy approach. Her postoperative course was uneventful until she had anemia one week after the surgery. Contrast-enhanced computed tomography showed right hemothorax due to bleeding from a branch of the right lateral thoracic artery. Endovascular coil embolization and gelatin sponge injection were performed. The patient was discharged without any complications on postoperative day 20.
INTRODUCTION
Bleeding from the thoracic wall is one of the major complications after minimally invasive mitral valve repair (MIMVR). Normally, this complication is found immediately after the operation, and re-exploration is required, while bleeding in the late phase is extremely rare. The first case of rare delayed thoracic wall bleeding after MIMVR, which was successfully treated by endovascular therapy (EVT), is presented.
CASE REPORT
A 55-year-old woman with asymptomatic severe mitral regurgitation (MR) was referred to our department for surgical evaluation. Transthoracic echocardiography showed severe MR (Barlow type) and moderate tricuspid regurgitation. Mitral valve repair (triangular resection, chordal translocation and annuloplasty with a 34-mm CG Future Annuloplasty Band (Medtronic, Inc., Minneapolis, MN, USA)) was performed through the fourth intercostal space with a mini-thoracotomy approach (no adhesion in the pleural space), similar to that previously reported [1]. Tricuspid valve repair using a 28-mm Physio Tricuspid annuloplasty band (Edwards Lifesciences, Irvine, CA, USA) was done concomitantly. Before wound closure, hemostasis of the incision and port insertion site was confirmed by endoscopy. The patient was extubated in the operating room, with stable hemodynamics. We started warfarin on postoperative day 3. The right chest drain tube was removed on postoperative day 4. One week after the surgery, her blood pressure dropped with anemia. PT-INR was 3.11 at this time. Contrast-enhanced computed tomography (CT) showed hemothorax on the right side. There was a tuberous enhancement in the right chest wall, and it was considered to be the bleeding source (Fig. 1). A chest drain tube was placed again and EVT was then performed. A catheter was inserted from the femoral artery to the right axillary artery, and extravasation of contrast medium from the right lateral thoracic artery was confirmed by angiography (Fig. 2). The microcatheter was inserted into the right lateral thoracic artery, and coil embolization (Hilal Embolizing Microcoil 2 mm × 2 cm, Cook Medical Inc., Bloomington, IN, USA) and gelatin sponge injection (Serescue, Astellas Pharma, Tokyo, Japan) were performed (Fig. 3a). Hemostasis was confirmed by postprocedural angiography (Fig. 3b). There were no EVT-related complications. The patient was discharged without any complications on postoperative day 20.
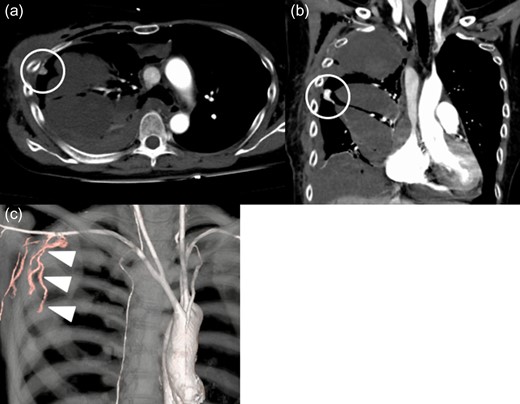
Contrast-enhanced computed tomography findings at 1 week. There is a tuberous enhancement in the right chest cavity near the fourth intercostal space (circle). Right lateral thoracic artery (arrow heads) connect to a tuberous enhancement. Axial view (a). Coronal view (b). Three-dimensional volume rendering computed tomography (c).
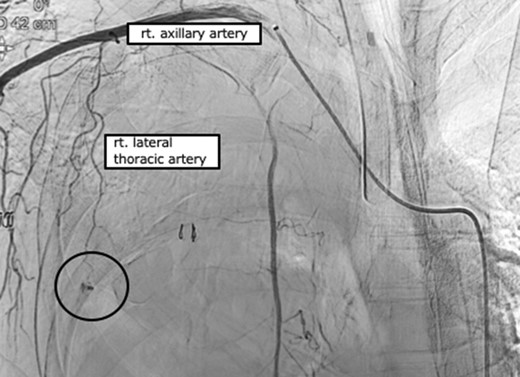
Angiography findings. Extravasation of contrast medium from the right lateral thoracic artery pseudoaneurysm (circle).

Angiography findings. Coil embolization with gelatin sponge injection for the right lateral artery pseudoaneurysm (arrowhead) (a). Extravasation from the right lateral thoracic artery has disappeared (b).
DISCUSSION
This is the first case report of delayed thoracic wall bleeding after MIMVR treated by endovascular therapy.
Recently, the minimally invasive approach has become the standard and preferred approach for mitral valve surgery, with excellent outcomes comparable to conventional sternotomy approach [2]. Even though MIMVR has comparable clinical outcomes, it has to be kept in mind that there are several MIMVR-specific complications, including leg ischemia, unilateral re-expansion pulmonary edema, stroke, and bleeding from the chest wall. Normally, these complications occur immediately after the operation and are treated then. In the present case, very rare thoracic wall bleeding occurred in the late phase. One of the benefits of MIMVR is early functional recovery and a shorter hospital stay. Atluri et al. reported that the mean hospital stay of MIMVR was 6 days, shorter than a sternotomy approach [3]. Therefore, it would be important to consider this late complication in the follow-up phase even after discharge, especially in patients with risk of bleeding (coagulopathy, antiplatelet use, etc).
Delayed hemothorax has been reported in chest trauma cases. It was found 2-14 days after the trauma, most frequently on the seventh day [4]. Counihan et al. reported delayed bleeding because of a traumatic pseudoaneurysm [5]. In the present case, despite the confirmation of hemostasis by endoscopy, the patient presented with hemothorax one week after the surgery. Considering the fact that the pseudoaneurysm was located at the edge of the incision, which was apart from chest tube (19Fr blake silicon drain, Ethicon, Inc., Somerville, NJ, USA) insertion site, the delayed bleeding might be caused by combination of increase in activity, confliction of costal bones and higher PT-INR value.
If postoperative bleeding is uncontrollable, re-exploration is needed. However, it may increase the risk of infection or lung injury. In the present case, we first considered surgical re-exploration, but CT identified the source of the bleeding precisely, and it was thought to be easily accessible by EVT. And the amount of hematoma in the right chest was thought to be controlled by chest tube drainage. Regarding EVT for chest wall bleeding, Pontell et al. reported that they could perform coil embolization for a lateral thoracic artery pseudoaneurysm due to penetrating chest trauma [6]. And EVT has other merits which are less invasive and lower risk of infection than re-opening the chest. Jeans et al. reported that Doppler ultrasound imaging provided possibilities for image-guided compression and direct injection of embolizing material for peripheral pseudoaneurysms [7].
To the best of our knowledge, this is the first case report of delayed massive thoracic wall bleeding after MIMVR treated by EVT. We need to keep in mind this rare late phase complication in the follow-up phase.
CONFLICT OF INTEREST STATEMENT
None declared.



