-
PDF
- Split View
-
Views
-
Cite
Cite
Aysha Rajeev, Faizan Jabbar, Jaganath Chakravarthy, Mike Newby, Isolated acute pisiform dislocation presenting atypically as wrist sprain in the emergency department, Journal of Surgical Case Reports, Volume 2019, Issue 6, June 2019, rjz183, https://doi.org/10.1093/jscr/rjz183
Close - Share Icon Share
Abstract
The pisiform is a sesamoid bone with in flexor carpi ulnaris tendon. Isolated dislocation of the pisiform bone is not common. It is usually missed and diagnosed as a soft tissue injury or a sprain of the wrist by the emergency physicians. We present an unusual and unique case of a young man involved in a rugby tackle and who himself presented to the emergency department with a painful wrist. The diagnosis of a dislocated pisiform was initially missed; however it was later successfully treated with an open reduction leading to a satisfactory outcome.Early diagnosis and reduction is imperative to avoid prolonged morbidity and loss of earnings. A high index of suspicion is needed in young patients with wrist trauma displaying ulnar sided wrist pain.
INTRODUCTION
The pisiform is a sesamoid bone located in the flexor carpi ulnaris tendon. Acute isolated dislocation of the pisiform bone is a rare and usually missed diagnosis in the emergency department [1]. They are often misdiagnosed as a sprain or soft tissue injury of the wrist by emergency physicians. This thereby delays the definitive diagnosis and required treatment. We report a case of an isolated, undetected dislocation of the pisiform bone treated with open reduction leading to a satisfactory outcome.
CASE REPORT
A 27-year-old male salesman, right hand dominant, was seen in the Emergency Department following a fall on to the outstretched hand while playing a game of rugby. He noticed immediate pain and swelling of the left wrist. Upon examination there was diffuse swelling on the dorso-medial aspect of the wrist. Tenderness was noted overlaying the ulna styloid process. He was non-tender to all scaphoid landmarks, metacarpals and phalanges. There was restricted range of motion of the wrist but full range of movements of the digits. There was no distal neurovascular deficit. The radiological examination of the left wrist was interpreted by the emergency doctors as no bony injury. A diagnosis of wrist sprain was made and was therefore treated with analgesia, ice application and a wrist splint as per local policy.
The X-rays of the patient was later reviewed by the duty radiologist and reported as a suspected dislocation of the pisiform bone, Fig. 1. Therefore the patient was recalled to the trauma clinic after three days. He was reassessed and a further three dimensional scan of the wrist was arranged. The CT scan demonstrated distal dislocation of the pisiform which appeared to lie in a ‘locked’ position beyond the distal triquetrum, Fig. 2.

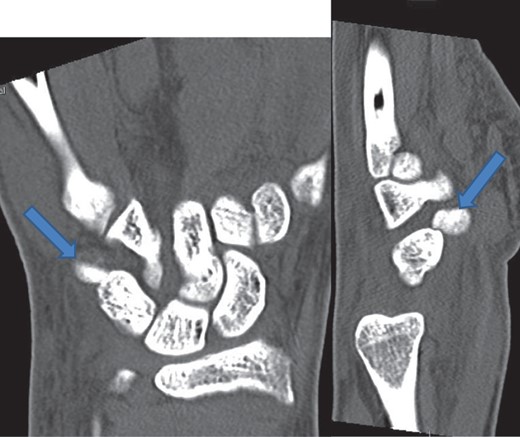
CT showing pisiform displaced from its anatomical position confirming dislocation.
The patient was taken to theatre the following day where a closed reduction of the dislocated pisiform was attempted, however it was unsuccessful. Therefore we then proceed to an open reduction. This was performed through a volar approach through the flexor carpi ulnaris tendon where the piso-hamate joint was exposed and a capsular release performed. This allowed the pisiform to reduce back in to the anatomical position Fig 3. The wrist was immobilized in a neutral position. The patient was followed up in the clinic in two weeks, six weeks, three and six months. The check X-ray performed at the end of six months demonstrated the pisiform remain well reduced, Fig 4. He subsequently regained full a range of motion within the wrist and was further discharged from the clinic.
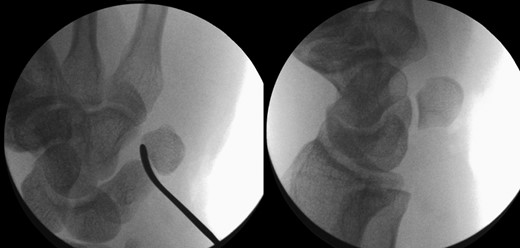
Image intensifier pictures showing reduction of dislocated pisiform bone.

Radiograph at 3 months showing pisiform bone anatomically reduced and maintained.
DISCUSSION
Isolated pisiform dislocation without other carpal bone injuries are rare and there are only a few case reports available in literature [2–5]. The anatomy of pisiform bone is unique. It is one of the proximal row carpal bones articulating with the triquetrum and hamate the articular surface of the pisiform bone is horizontal. The primary stabilizers are flexor carpi ulnaris (FCU) tendon, ulnar pisotriquetral ligament, pisometacarapal and pisohamate ligament [6]. The FCU is attached to the anterior aspect of the pisiform bone. When the FCU contracts it pulls the pisiform proximally and with the help of pisohamate and pisometacarpal ligaments it aids in wrist flexion [7].
There are two mechanisms postulated that can cause an acute pisiform dislocation. The first mechanism is a direct force applied to the pisiform bone. The second mechanism is an indirect force due to hyperextension of the wrist with strong contraction of the FCU displacing the pisiform more proximally and thus causing a dislocation [3, 4]. With our patient it was the second mechanism caused by a fall on the out stretched hand causing hyperextension of the wrist with a violent pull of the FCU thus causing dislocation of the pisiform bone.
The clinical diagnosis of pisiform dislocation is usually dependant on the injury mechanism and the presence of pain, swelling and tenderness over the ulnar aspect of the wrist. Our patient had pain, swelling and tenderness in the dorso-medial aspect of the wrist. The radiographs may not be able to demonstrate the dislocation of the pisiform in a standard AP and lateral views. An oblique radiograph and comparison with the contralateral side is quite often helpful. Computer tomograms are conclusive and Magnetic Resonance imaging will show the associated ligamentous and soft tissue injuries. In our patient the emergency physicians failed to diagnose the dislocation of pisiform in the initial radiographs, but CT scan confirmed the diagnosis.
The treatment options are closed manipulative reduction and immobilization, open reduction and internal fixation and resection of the pisiform bone. There are different views regarding the immobilization of the wrist after closed manipulative reduction. In their report Ishizuki et al. described that after closed reduction, the stability of the pisiform, is dependent on the wrist position in which it is immobilized [8]. Minami et al. reported a redislocation after 3 months of immobilization in 20 palmar flexion of the wrist and the neutral position of forearm [4]. The forearm to be in a full pronation so that the FCU will be in a full relaxed position [5].In our patient the wrist was immobilized in neutral position.
Open reduction and internal fixation is indicated when the closed reduction is unsuccessful and the diagnosis is delayed [3, 4]. The late sequelae of a missed dislocation of the pisiform are recurrent dislocations, persisting pain and development of pisohamate or pisotriquetral arthritis [9, 10].
Wrist injuries are one of the most common conditions seen in the emergency department. In a young patient with atypical presentation of ulnar sided wrist pain after an injury, a differential diagnosis of pisiform dislocation should be considered. A prompt and immediate referral to the orthopaedic doctor on call should be carried out so that early diagnosis and correct treatment can be instigated.
CONFLICT OF INTEREST STATEMENT
None declared.



