-
PDF
- Split View
-
Views
-
Cite
Cite
Chi-Man Yip, Huai-Pao Lee, Pin-Pen Hsieh, Pituitary spindle cell oncocytoma presented as pituitary apoplexy, Journal of Surgical Case Reports, Volume 2019, Issue 6, June 2019, rjz179, https://doi.org/10.1093/jscr/rjz179
Close - Share Icon Share
Abstract
Spindle cell oncocytoma is a rare nonfunctioning neoplasm of the adenohypophysis, and was first described in 2002 by Roncaroli et al. In 2007, spindle cell oncocytoma has been categorized as a separate entity by the World Health Organization (WHO) and is classified as a Grade 1 tumor of the central nervous system. Spindle cell oncocytoma of pituitary gland usually occurs in adults and accounts for 0.1–0.4% of all sellar region tumors. Clinically and radiologically, they are indistinguishable from nonfunctioning pituitary adenomas. From 2002 to 2018, approximately 46 cases of spindle cell oncocytoma of pituitary gland had been reported in the English literature and we would like to report a case of 28-year-old woman presented with pituitary apoplexy proved to be a case of spindle cell oncocytoma of pituitary gland which probably will be the 47th reported case.
INTRODUCTION
Spindle cell oncocytoma is a rare nonfunctioning neoplasm of the adenohypophysis, and was first described by Roncaroli et al. [1] Roncaroli et al. defined spindle cell oncocytoma as spindled in appearance, with eosinophilic granular cytoplasm and numerous swollen mitochondria, immunoreactivity for vimentin, epithelial membrane antigen (EMA), galectin-3, and S-100 protein, but negative stains for pituitary hormones, synaptophysin, chromogranin, glial fibrillary acidic protein, cytokeratin CAM5.2, smooth muscle actin, CD34 and CD68. Through the view of the electron microscope, the tumor cells contained numerous mitochondria with lamellar cristae and were linked by intermediate junctions and desmosomes; secretory glandules were not detected [1]. Spindle cell oncocytoma has been categorized as a separate entity by the World Health Organization (WHO) in 2007 and is classified as a Grade 1 tumor of the central nervous system (CNS) due to its low proliferative activity and less invasiveness [2, 3]. From 2002 to 2018, only 46 cases of spindle cell oncocytoma of the pituitary gland have been reported [2, 3]. We would like to report a case of spindle cell oncocytoma to present with pituitary apoplexy. Pituitary apoplexy is characterized by sudden increase in pituitary gland volume due to acute infarction and/or hemorrhage, usually in a pituitary adenoma. As a result of an abrupt increase of tissue volume within the sellar region, it can cause headache, visual impairment, cranial nerve palsies and conscious disturbance due to mass effect [4, 5]. Pituitary apoplexy is an uncommon clinical syndrome, which complicates 2-12% of pituitary adenomas [5]. The precise pathophysiology is not yet completely understood; some precipitating factors have been identified. These trigger factors include vascular flux reduction, acute increase in blood flow, pituitary stimulation, coagulation disturbance, dopamine agonist therapy, head trauma [4, 5]. Pregnancy is a risk factor for pituitary apoplexy, probably due to an increased pituitary volume due to lactotroph hyperplasia and increased pituitary blood flow induced by estrogens [4].
CASE REPORT
In May 2018, a 28-year-old woman with medical history of sick sinus syndrome and mitral valve prolapse, who just gave birth to a child in April 2018 coming to our Emergency Department with the chief complaint of severe headache and blurred vision for one week. At the Emergency Department, her visual acuity was 0.1 on her right eye and 0.9 on her left eye. Brain CT (computed tomography) scan was checked showing increased soft tissue density over sellar and suprasellar regions, more on the right side. Sellar MRI (magnetic resonance imaging) (Fig. 1) was further arranged which showed a mass with rim enhancement about 2.2 cm ×1.4 cm ×1.2 cm in size located at sella with suprasellar extension with several suspected hemorrhagic foci inside. Under the impression of pituitary apoplexy, she was admitted for further evaluation and management. On admission, her neurological examination showed essentially negative findings except declined right visual acuity; her hormone study showed low level of cortisol (cortisol<1.00 μg/dL) and others were within normal limits. Before surgery, ophthalmologist was consulted again to repeat her ophthalmological examination. The visual acuity of her right eye and left eye improved to 0.8 and 1.0 respectively after the use of steroid. The visual field test showed peripheral defect over the upper visual field of both eyes. Under general anesthesia, she underwent endoscopic endonasal transsphenoidal approach with the removal of tumor and skull base reconstruction. Grossly, the tumor was yellow and soft in consistency and at the end of the procedure, the pituitary gland was well exposed and visible (Fig. 2). After surgery, her vision was subjectively improved; her cortisol level returned to normal (cortisol=16.6ug/dL) and other hormonal data were within normal limits. Histology examination of the tumor (Fig. 3) showed that it composed of spindle to epithelioid cells forming poorly defined lobules and interlacing fascicles, both featuring eosinophilic and oncocytic cytoplasm, with mild nuclear atypia. Immunohistochemically, the neoplastic cells showed TTF-1(+), GFAP(-), EMA(+) Annexin A1(+), and PAS/DPAS(-). Based on the result of histopathology findings and immunohistochemical stains, spindle cell oncocytoma was diagnosed. Before discharge home, her early post-operative sellar MRI (Fig. 4) showed neither residual nor recurrent lesion; she was discharged in a good condition.
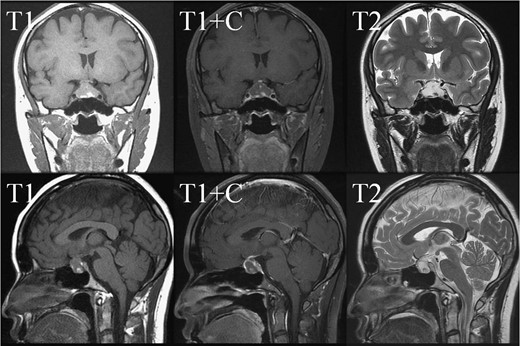
Pre-operative sellar MRI. The coronal view (upper row) and sagittal view (lower row) demonstrated a mass about 2.2 cm ×1.4 cm ×1.2 cm in size, located at sella with suprasellar extension. The mass lesion showed low intensity in T1 weighted image, high intensity in T2 weighted image, and rim enhancement after gadolinium injection. Inside the mass, several foci showing high intensity in T1 weighted image, low intensity in T2 weighted image and no enhancement after gadolinium injection were present.
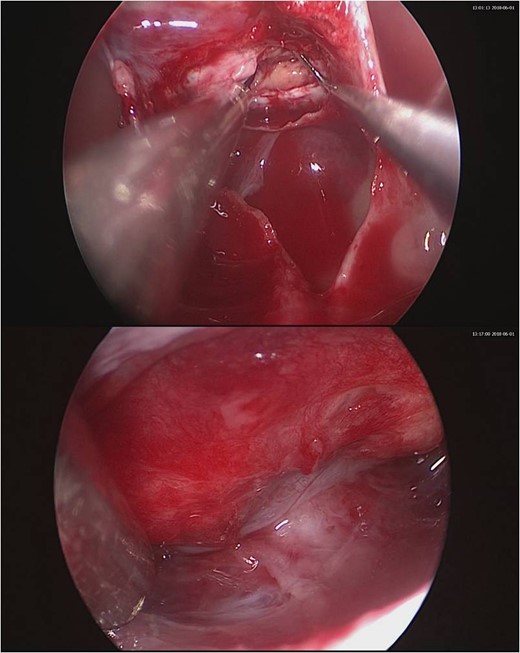
Intraoperative pictures. Upper one showing the gross appearance of the tumor. Lower one showing the normal pituitary gland after tumor removal.
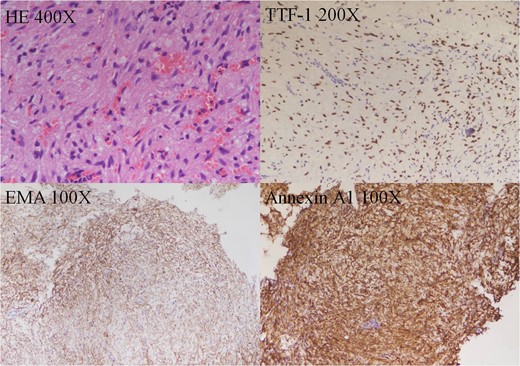
Histology of the tumor. HE stain showing it composed of spindle to epithelioid cells forming poorly defined lobules and interlacing fascicles, both featuring eosinophilic and oncocytic cytoplasm, with mild nuclear atypia. Immunohistochemically, the neoplastic cells showed TTF-1(+), EMA(+) Annexin A1(+).
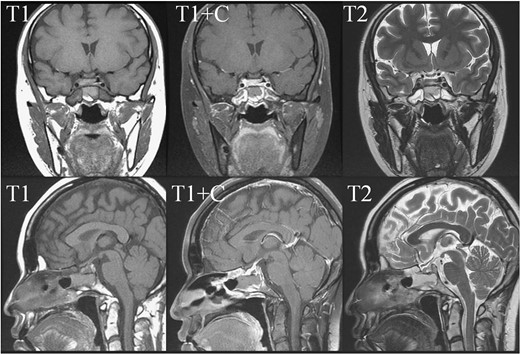
Early post-operative sellar MRI. The coronal view (upper row) and sagittal view (lower row) showing the status post removal of the tumor over the sellar and suprasellar regions with poor-enhancing area at the posterior sellar region which favored postoperative change.
DISCUSSION
Spindle cell oncocytoma is a recently described distinct pituitary benign neoplasm which usually occurs in adults and accounts for 0.1–0.4% of all sellar region tumors [3]. Clinically and radiologically, they are indistinguishable from nonfunctioning pituitary adenomas [1–3]. Based on similar immunohistochemistry (positive stain for S-100 protein) and ultrastructural features (the presence of desmosomes and gap junctions), an origin from folliculostellate cells has been suggested [1, 3]. Folliculostellate cells are agranular cells located in the parenchymal tissue of the anterior pituitary gland and thought to act as adult stem cells of pituitary, capable of divergent differentiation [3, 6]. In 2013, Mete et al., reported TTF-1 expression in spindle cell oncocytoma, pituicytomas, and granular cell tumors; however, all were negative for markers of folliculostellate cells [7]. They hypothesized that spindle cell oncocytoma, pituicytomas, and granular cell tumors may have an origin in the pituicyte, and that spindle cell oncocytoma may be a variant of pituicytoma [3, 7].
From 2002 to 2018, approximately 46 cases of spindle cell oncocytoma of the pituitary gland have been reported in the English literature [2, 3]. Visual disorder, hormonal disorder and headache were the major clinical features of these 46 patients. Other clinical presentations included conscious disturbance, memory loss, epistaxis; one patient detected the lesion incidentally [2, 3]. The most common clinical manifestations of spindle cell oncocytoma are visual impairment, headache and hormonal disorder due to mass effect [3]. Surgical resection is the treatment of choice. Long-term aggressive regular follow-up is recommended due to higher recurrent and progression rate of this tumor as compared to other pituitary adenoma [2, 3]. Back to our patient, pregnancy and parturition probably were the trigger factors for her pituitary apoplexy. Because of the tumor location and the sudden increase of tumor volume due to bleeding, visual disorder and headache were resulted. Certainly, we did not expect she got this unusual tumor before surgery.
CONFLICT OF INTEREST STATEMENT
We report no conflicts of interest.



