-
PDF
- Split View
-
Views
-
Cite
Cite
Mario Antunes, Damiano Pizzol, Mattia Zambon, Anna Claudia Colangelo, Giant ovarian fibroma with associated Meigs syndrome in low resources setting, Journal of Surgical Case Reports, Volume 2019, Issue 4, April 2019, rjz143, https://doi.org/10.1093/jscr/rjz143
Close - Share Icon Share
Abstract
Meigs' syndrome is a rare condition characterized by the presence of a benign fibroma of the ovary, ascites and pleural effusion. It very uncommon and diagnosis is made difficult by symptoms that usually mimic disseminated malignancy. The gold standard treatment is laparotomy and, by definition of the syndrome, after tumor removal, the symptoms resolves and the patients become asymptomatic. We presented a giant ovarian fibroma with associated Meigs syndrome, successfully managed in a low resources setting.
INTRODUCTION
Meigs' syndrome is a rare condition defined by the presence of a benign fibroma (or a fibroma-like tumor) of the ovary, ascites and pleural effusion [1]. If just ascites or pleural effusion is present, it is defined as incomplete or pseudo Meigs' syndrome [1]. The peculiar characteristic is the reabsorption of the excess fluid after the surgical resection [2]. It is very uncommon before the third decade and the incidence progressively increases with age with a peak in the seventh decade with a prevalence of about 1% of ovarian tumors [3]. Our knowledge on Meigs’ Syndrome comes mainly from case reports and according to Krenke et al. is it possible to identify five patterns of the disease: Classic Meig’s syndrome, nonclassic and demons-Meig’s syndrome, pseudo Meigs’ syndrome, Pseudo-Pseudo Meigs’ syndrome, Atypical or incomplete Meigs’ syndrome [4]. All the patterns are characterized by ascites, pleural effusions and the resolution of both ascites and hydrothorax after tumor removal. Each pattern, well described by Krenke and colleagues, has a specific type of tumor that allows the differentiation from the other ones [5]. In particular, patients without a known prior diagnosis of systemic lupus erythematosus often present the combination of mild to moderate ascites, pleural effusion and elevated serum carbohydrate antigen 125 concentration; the onset is gradual and painless [5, 6].
We presented a giant ovarian fibroma with associated Meigs syndrome, successfully managed in a low resources setting.
CASE PRESENTATION, MANAGEMENT AND OUTCOME
A 41-year-old woman presented in Beira Central Hospital, Mozambique, with a giant abdominal mass, evolved over about four years (Fig. 1A and B). The patient presented with pain and abdominal distension, feeling of weight, discomfort and slight weight loss. She reported four pregnancies including three regular and one stillborn. She was HIV positive, on ART with tenofivir/lamivudine/efavirenz from four years. Four years before, at the beginning of the disease, she underwent an explorative laparotomy. In that occasion, colleagues decided to not remove the mass and just a bioptic specimen was collected and the histological diagnosis was suggestive for an ovarian cyst. One year before other colleagues decided to perform a second biopsy and it was suggestive for calcific fibroma. Finally, we decide to remove the whole mass. Her general condition was good, and she had normal vital parameters. Hepatic and renal functions were normal and blood test showed Hb 9 g/dl Ht 33.4% PLT 405 × 103 CD4 233 cell/ul. We performed a transversal supra-umbilical laparotomy removing an abdominal mass of about 10 kg (27 × 30 × 20 cm) (Fig. 1C and D) and 10 liters of free fluid liquid like ascites. The abdominal mass originated from the ovary and was strictly adherent to the bowel thus necessitating to perform bilateral hysteroadnexiectomy and enbloc resection of more or less 60 cm of bowel, including ileocecal valve, with termino-terminal ileotransverse anastomosis. During surgery, there was an important blood loss that required three unit of blood and three unit of plasma due to anemia with hemoglobin of 3.5 g/dl. During post-operative course, it was also necessary to transfuse other three unit of blood and fluid infusion. Histological diagnosis was ovarian fibroma and leiomyoma uteri. During the post-surgical course, we administrated antibiotics and analgesic treatment. She was discharged in 15 days and after 2 years post-surgery the patient is alive, apparently with no sequela.
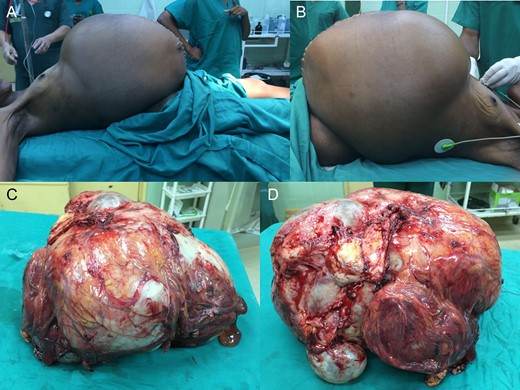
Giant incomplete Meigs’ syndrome at presentation (A and B) and the excised mass (C and D).
DISCUSSION
Meigs' syndrome pathophysiology, both in terms of ascites and hydrothorax formation, is still unknown and among several theories, two received major consensus. One suggests that the filtration of interstitial liquid into the peritoneum through the ovarian tumor capsule with an imbalance between the blood supply to a large tumor leading to edema and transudation [4]. Thus, liquid moves from peritoneum to pleural cavity both through diaphragmatic defects or lymphatic channels causing pleural effusion [3, 7]. The other suggests a fluid accumulation caused by proteins such as vascular endothelial growth factor raising capillary permeability [8]. The most common presenting symptoms are dyspnea (due to pleural effusion), fatigue and weight loss and most of the patients initially referred to the general practitioner or chest physicians [5, 9]. However, considering that the ovarian pathology is the benign disease, symptoms usually strongly mimic disseminated malignancy. The treatment of choice of Meigs' Syndrome is exploratory laparotomy and, by definition of the syndrome, after tumor removal, the symptoms resolve and the patients become asymptomatic [1, 10]. Paracentesis and thoracentesis are a possible treatment for ascites and pleural effusion [3]. Life expectancy of patients after surgical removal of the tumor is the same as the general population [3].
Usually, in low- and middle-income countries extreme presentations of late-stage diseases occur due to the weaknesses of healthcare systems and also due to cultural and economic reasons. Besides the belated presentation of the patient, a big issue was to perform a correct diagnosis. In fact, the two main diagnostic tools, computed tomography, and oncological markers are not available at our hospital. Moreover, X-ray was not performed and we are not able to confirm if it was an ovarian fibroma with associated complete or incomplete Meigs’ syndrome. Again, due to the lack of specialized health workers and equipment, in this case, the lady underwent two surgical biopsies before the radical intervention. However, despite the low-resource setting and the extreme disease condition, a surgical procedure was performed successfully. The second crucial issue is related to follow-up that should be regular especially for oncologic patients. However, due to the difficult access to the hospital, the important role of traditional healers and the lack of health education, it is rare to follow-up patients. In our case, we know that the patient is still alive after about two years because we meet her out of work, but we don’t know if she has some recurrence of ascites or abdominal mass.
Our case reports a very rare syndrome case and highlights the weakness of the health system of low-income countries. It is mandatory to strengthen the health system, both in terms of healthcare and prevention.
CONFLICT OF INTEREST STATEMENT
The authors have not conflict of interest to declare for this work.
COMPLIANCE WITH ETHICAL STANDARDS
Written informed consent was obtained from the patients for publication of this case report and any accompanying images.
FUNDING SOURCE
None.



