-
PDF
- Split View
-
Views
-
Cite
Cite
Yi Liang, Angelina Di Re, Toufic El Khoury, A rare case of lupus-related gastrointestinal vasculitis presenting as rectal gangrene, Journal of Surgical Case Reports, Volume 2019, Issue 4, April 2019, rjz128, https://doi.org/10.1093/jscr/rjz128
Close - Share Icon Share
Abstract
Systemic lupus erythematosus (SLE) related gastrointestinal vasculitis is a rare condition limited to case studies within the literature however, no cases of rectal gangrene and perforation have been previously described. A 32-year-old male presented with abdominal pain, vomiting and fevers. CT demonstrated free gas and free fluid around the rectum indicative of a perforation. He proceeded to urgent laparotomy, confirming a diagnosis of rectal infarction and perforation. Uniquely, the involved segment of gangrene extended from the rectosigmoid to the anorectal junction. A Hartmanns procedure was performed. Histopathology confirmed underlying stenosis of the rectal arteries secondary to chronic vasculitis related to the affected areas. The current case is a unique presentation of SLE-related vasculitis. It highlights the need to judiciously investigate SLE patients presenting with surgical acute abdomen.
INTRODUCTION
Systemic lupus erythematosus (SLE) is an autoimmune condition associated with a generally accepted <1% incidence of gastrointestinal vasculitis (though some studies quote as high as 53%) [1, 2]. Those affected by gastrointestinal vasculitis tend to be male and have a higher baseline disease activity [2]. Though rare, ischaemic colitis and perforation are manifestations of small vessel vasculitis [3, 4]. However, few cases of SLE-related rectal disease exist in the literature as the rectum is considered to have redundant vasculature [3]. The management of SLE-associated colitis with glucocorticoids remains the mainstay of treatment. Surgical resection is reserved for cases of perforation and sepsis [2, 5]. We present a case of acute rectal gangrene associated with SLE-related vasculitis requiring an urgent surgical resection and formation of end colostomy.
CASE STUDY
A 32-year-old man presented acutely to a regional hospital with left sided abdominal pain and loose bowel motions. He had a known history of chronic SLE colitis demonstrated on colonoscopy several years previously. He had experienced rectal bleeding a fortnight prior, which was attributed to be due to SLE colitis, and was treated with increased oral prednisolone dose with a pending referral for colonoscopy. He previously had received courses of mycophenolate and rituximab. His current maintenance therapy was a combination of prednisolone and hydroxychloroquine. He also had been diagnosed with other SLE-related vasculitis manifestations including Cerebral Lupus and Lupus Nephritis.
In the regional hospital, the patient had progressive peritonitis and vomiting. He was tachycardic and febrile (Temp 38.5°C). His initial work up demonstrated urea 11.9 mmol/l, creatinine 121 umol/l, C-reactive protein 201 mg/l, white cell count 30.7 × 109/l and haemoglobin 112 g/l. An urgent CT abdomen and pelvis demonstrated a large amount of free gas in the perirectal space consistent with a rectal perforation (Figs 1–3). The rectum itself was thick-walled and oedematous, as well as the sigmoid colon. He was transferred to the referral Tertiary hospital where an urgent laparotomy was performed.

CT axial. Free gas within the pelvis around the rectum as well as pneumointestinalis of the rectum suggestive of ischaemia and perforation.
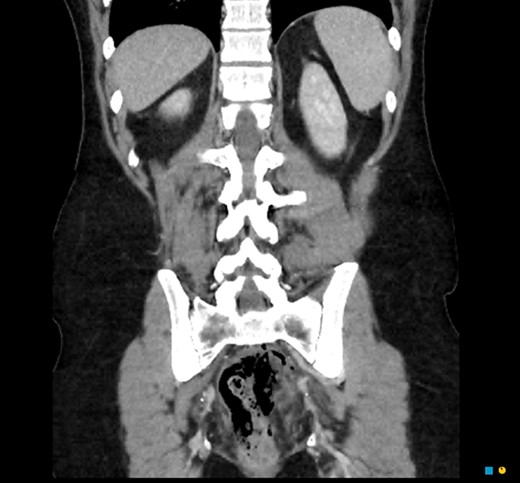
CT coronal. Pneumointestinalis of the rectum suggestive of perforation.

CT sagittal. Large amount of perirectal free gas consistent with rectal perforation. The rectum is thick-walled and oedematous suggestive of ischaemia.
An exploratory laparotomy demonstrated the entire length of the rectum (from the anorectal junction to sigmoid) was necrotic with several points of perforation (Fig. 4), thus an ultra-low anterior resection was performed. An omental wrap was placed into the remaining pelvic defect and an end colostomy was fashioned from the remaining sigmoid colon. Significantly, there appeared to be no macroscopic evidence of disease to the remaining colon and small bowel. He was admitted to the ICU post-operatively and was gradually weaned from ionotropic support and ventilation, as he also overcame his comorbid aspiration pneumonia. He completed seven days of IV Piperacillin and Tazobactam as well as IV stress doses of hydrocortisone.
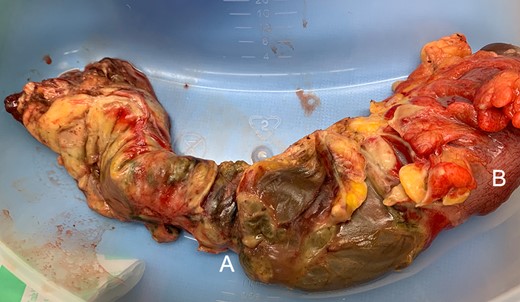
(A) Rectal gangrene with multiple sites of perforation. (B) Healthy rectosigmoid at proximal resection margin.
Histopathology demonstrated ischaemic rectum with patches of transmural infarction. This seemed to be superimposed upon areas of chronic colitis where the usual mucosal crypt architecture was distorted. Significantly, the small mesocolonic vessels appeared abnormal. The arteries had marked hyperplasia resulting in severe stenosis (Fig. 5). In areas of infarction, these vessels demonstrated acute vasculitis with mural necrosis and fibrinous inflammation (Fig. 6). These vasculitis changes were not reflected in viable, non-inflamed submucosa and mucosa. Tissue at the resection margins demonstrated mucosal ulceration but viable bowel wall.
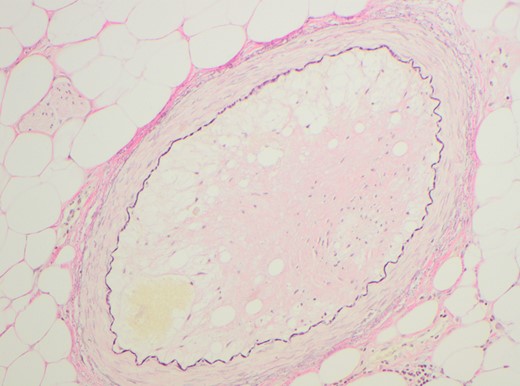
Elastin highlighting the internal elastic lamina (IEL). Elastin confirms luminal narrowing secondary to intimal thickening.
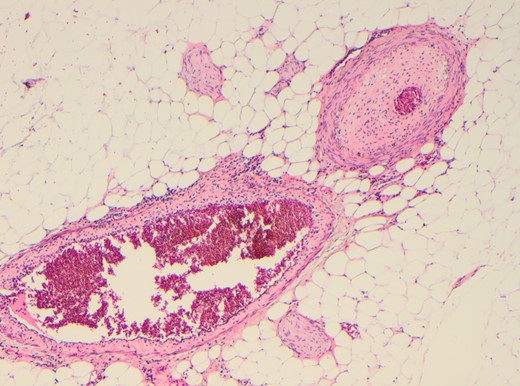
Marked arterial luminal stenosis and marked thickening of intima. The adjacvent small vein also demonstrates transmural phlebitis and slight thickening of its intima.
The patient made a full recovery by Day 12 of admission and was subsequently discharged.
DISCUSSION
Vasculitis is a rare complication of SLE, it can affect any segment of the gastrointestinal tract [2]. Progressive vasculitis leads the luminal stenosis of small end vessels. Detection is difficult; clues of disease progression can be found in our patient’s previous diagnosis of chronic colitis and rectal bleeding. In retrospect, this may have been a ‘herald bleed’. Diagnostic angiography has been utilized previously in the detection of large and small vessel disease related to SLE vasculitis [5]. Previous cases of vasculitis-related colitis have pointed to the relative sparing of the rectum and this has been postulated to be the result of the rectum’s redundancy in vascularization [6, 7]. The current case is unique as only the rectum was involved.
The incidence of SLE-related gastrointestinal vasculitis is variable [8], making diagnosis difficult. Patients can present with variable symptoms including non-specific abdominal pain and diarrhoea, which may reflect non-vasculitis related SLE gastrointestinal manifestations (for example, pancreatitis). Therefore, patients with known SLE, particularly those with previously diagnosed with SLE vasculitis, should be investigated thoroughly. CT scans are integral to the non-invasive assessment of bowel loops and intestinal blood supply. Ascitic free fluid, bowel wall thickening (often multi-segmental), abnormal bowel wall enhancement (halo sign), mesenteric oedema and vessel engorgement are all indicators of ischaemic bowel [9]. Detection rates of the underlying vasculitis related ischaemia in patients presenting with SLE-related abdominal pain can be high as 79% [9].
Few cases of SLE-related rectal necrosis exist in the literature; treatment is often determined by clinical progression. Cases of ischaemic colitis managed with steroids and non-operative management have been described [6]. However, in the current case, the extent of necrosis and progressive sepsis required aggressive and expedient surgical control. Patients who present with an acute surgical abdomen, as in the current case, represent a high morbidity and mortality risk for patients with SLE with mortality rates of 39% (14 of 36 cases) in patients with active SLE presenting with acute abdomens [1]. Unique to the current case was the extent of necrotic involvement necessitating a resection of the entire rectum to the anorectal junction [10]. Described a case of ischaemic transverse colonic perforation requiring an oversew and colostomy formation though the full extent of mucosal involvement of colonoscopy was diffuse throughout the colon [10]. In the current case, we advocated for a more aggressive resection given the difficulty of accessing the area of necrotic perforation within the pelvis as well as the extent of necrotic involvement. The demarcation of necrotic disease allowed for the preservation of the anus.
CONCLUSION
SLE-related gastrointestinal vasculitis is a rare entity, however correlates with acute abdominal pain presentations. Patients with known SLE-related vasculitis should be investigated thoroughly with a high index of suspicion for bowel ischaemia. Expedient and judicious surgical intervention is crucial.
Conflict of Interest statement
None declared.
Disclosure
The authors report no proprietary or commercial interest in any product mentioned or concept discussed in this article.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors
Author Contributions
Dr Yi Liang, Dr Angelina Di Re and A/Prof Toufic El Khoury all contributed equally to the collection of data and composition of the manuscript.
References



