-
PDF
- Split View
-
Views
-
Cite
Cite
Engida Abebe, Abebe Megersa, Kirubel Abebe, Huge thyroglossal duct cyst at the supra-sternal notch, Journal of Surgical Case Reports, Volume 2019, Issue 4, April 2019, rjz112, https://doi.org/10.1093/jscr/rjz112
Close - Share Icon Share
Abstract
Thyroglossal duct cysts (TGDC) are the most common congenital cysts in the neck. TGDC typically present as a midline swelling anywhere between the foramen cecum and the isthmus of the thyroid gland. Majority occurs just below the hyoid bone and those descending below the thyrohyoid membrane are rare. TGDC are usually less than 3 cm in diameter while big cysts are uncommon. We present a 19 years old female patient who presented with giant (12 cm diameter) supra-sternal notch cyst which was diagnosed as TGDC only after histopathology. The rarity of such huge TGDC in such uncommon site, which was misdiagnosed as a retention cyst (Mucocele) made us report this case.
INTRODUCTION
Thyroglossal duct cysts (TGDC) are the most common congenital cysts in the neck [1, 2]. A thyroglossal duct cyst arises as a cystic expansion of a remnant of the TGD anywhere between the foramen of cecum and the isthmus of the thyroid. Many cystic remnants of the thyroglossal tracts are never detected clinically. Nevertheless, a postmortem study shows 7% incidence of TGDC [3]. It occurs almost equally in both male and female [1, 3].
TGDC usually causes no symptoms, but may be slightly tender. Often the patient has or recently had an upper respiratory tract infection. Whether the infection leads to cyst formation or simply increases the likelihood of detection of a preexisting cyst is uncertain [1].
TGDCs are found within 2 cm of the midline, but can be somewhat more lateral and may even be lateral to the thyroid cartilage (more typically on the left) [4]. The typical cyst does, however, maintain a close relationship to the hyoid, thyrohyoid membrane, or thyroid cartilage [1, 2]. Here, we present a 19 years old female patient who presented with a huge supra-sternal notch lump which was later proved to be TGDC by histopathology. The rarity of such huge cyst in such uncommon site made us report this case.
THE CASE
A 19-year-old female patient from the rural Ethiopia presented with supra-sternal notch swelling. She had the swelling since she can remember but showed rapid growth in the last three years. She had mild pain which get worse in episodes of URTI. She did not have hyperthyroidism or hypothyroid symptoms.
On examination, she had a huge non-tender supra-sternal anterior neck cystic swelling measuring 12 cm in its biggest diameter and moves with swallowing. Related to the size, it was difficult to tell if it moves with protrusion of the tongue. (Fig. 1). No abnormalities detected in other systems examination. On investigation, complete blood count was normal while neck ultrasound showed a well-circumscribed supra-sternal heterogeneous cystic mass and normal thyroid in its position. Fine needle aspiration cytology (FNAC) report was a retention cyst (Mucocele). Thyroid function tests were in the normal range.
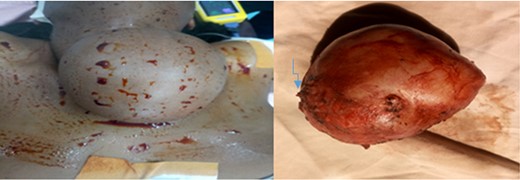
The cyst, preoperative (left) and a excised cyst with atrophied stamp (the arrow, right).
Intra-operatively the cyst was found to extend from the hyoid bone to the supra-sternal notch crossing anterior to the isthmus of the thyroid. Complete excision of the cyst was done. Examination of the excised specimen revealed an atrophied pedicle like extension in its proximal end, arrow in Fig. 1. The possibility of TGDC was entertained and the tissue subjected for histopathology. The pathology slides showed a fibro-collagenous cyst lined by simple cuboidal to columnar epithelium with areas of mononuclear inflammatory infiltrates within the stroma featuring TGDC. (Fig. 2) Patient discharged in the first post operative day and was on regular follow up after wards. After the pathology result the patient was counseled for possible development of Thyroglossal fistula and was on regular follow-up. Six months after the surgery the patient didn’t have signs of thyroglossal duct fistula.
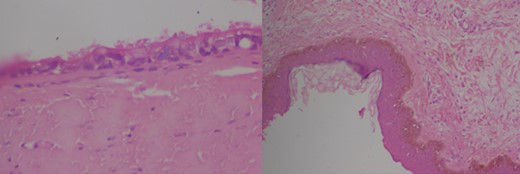
Pathology slides of the specimen confirming the diagnosis of TGDC (high and low power magnification).
DISCUSSION
Anterior neck swellings are among the common complaints a general surgeon sees at his regular OPD, which is mostly a goiter. Cysts in the neck are not uncommon [1–3, 5]. In goiter endemic areas cystic degenerations of a MNG is the most common finding. Among true cysts, TGDC is the most commonly seen cyst in the neck, especially in the first decade of life [1, 2]. Seeing TGDCS in the late second decade of life or later, like in our patient, is a rarity. The other cysts in the neck include dermoid/epidermoid cysts, brachial cysts, lymphangiomas, hydatid cyst, etc… [2].
TGDC are typically small in size(less than 3 cm in diameter) and can occur anywhere in the direction of descent of the thyroid form the foramen of cecum. Most (more than 85%) of the TGDC are in close relationship with the Hyoid bone [1]. Though huge TGDC close to the hyoid bone has been reported, a cyst reaching to the supra-sternal notch is rare [4, 6].
Masses or cysts in the supra-sternal notch can be easily confused with goiter as the later is the most frequent form. Our patient not only had the TGDC in unusual site, but also uncommonly huge cyst. The size is a likely explanation why it was below the thyroid i.e. when the cyst progressively enlarges it can grow anterior and below the isthmus of the thyroid gland as seen in our patient during the surgery.
The standard of care for patients with TGDC is Sistrunk’s operation, which is removing the cyst with the body (central part) of the Hyoid bone and ligation of the duct at the foramen of cecum [5, 7]. Because our patient’s diagnosis was a retention cyst a simple excision of the cyst was done. Clinical, sonographic and Cytology evaluation missed the diagnosis due to the rarity of the condition in that location and inconclusive investigation results.
After learning the diagnosis of the TGDC by histopathology we were considering the possibility of the patient developing Thyroglossal duct fistula which can occur in as high as 85% cases when Sistrunk’s operation was not done [5, 7]. Fortunately the patient didn’t develop it at least in the first 6 months post op. This could be just early (relatively short) post operative course or might have to do with fibrosis of the proximal duct from recurrent infection and scarring which could resulted in obliteration of the duct. Considering TGDC in the list of the differential diagnosis is crucial to avoid making the same mistake like us.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
Ali I. Swaid, Ahmed Y. Al-Ammar.



