-
PDF
- Split View
-
Views
-
Cite
Cite
Jacqueline Bakhit, Benjamin Privett, Nezor Houli, Laparoscopic trans-cystic common bile duct stone retrieval in a patient with gallbladder agenesis, Journal of Surgical Case Reports, Volume 2019, Issue 3, March 2019, rjz094, https://doi.org/10.1093/jscr/rjz094
Close - Share Icon Share
Abstract
Gallbladder agenesis is a rare but well-documented anatomical variation. Pre-operative diagnosis may be difficult as patients can present with typical symptoms of biliary colic and imaging may be misleading. We report a case of choledochoscopy and common bile duct stone retrieval in a patient found to have agenesis of the gallbladder intra-operatively.
INTRODUCTION
Gallbladder agenesis is a rare but well-documented anatomical variation, with an incidence of between 10 and 65 cases per 100 000. Despite the absence of the gallbladder, some patients may still present with typical symptoms of biliary colic [1]. Symptoms are more common in women, although the incidence of gallbladder agenesis is equal amongst men and women [2]. Many of these patients proceed to surgical intervention based on misleading ultrasonography demonstrating a shrunken gallbladder, suggestive of chronic cholecystitis [3].
There have been multiple cases of gallbladder agenesis reported, many of which have been diagnosed at time of laparoscopy and laparotomy [1, 4]. The authors report a case of successful choledochoscopy and common bile duct (CBD) stone retrieval in a patient found to have gallbladder agenesis at time of laparoscopy and the difficulties of pre-operative diagnosis.
CASE REPORT
A 69-year-old man presented to the emergency department with three days of right upper quadrant and epigastric pain, jaundice and nausea. He had no previous abdominal surgeries.
On examination he was found to be jaundiced, with right upper quadrant tenderness. He had a negative Murphy’s sign. Liver function tests demonstrated a bilirubin of 154 umol/L, with an alanine transaminase of 732 U/L, aspartate transaminase of 448 U/L, alkaline phosphatase of 244 U/L and gamma-glutamyl transferase of 636 U/L. He was placed on intravenous ceftriaxone and metronidazole while awaiting imaging.
Transabdominal ultrasound of the biliary tract was limited by bowel gas but reported an impression of multiple stones in the region of the gallbladder. The CBD was measured at 7 mm but was not entirely visualized and intrahepatic ducts were dilated up to 5 mm.
The patient then proceeded to have a magnetic resonance cholangiopancreatography (MRCP) scan for further assessment of the biliary tree. This demonstrated choledocholithiasis within the distal CBD measuring 5.9 mm. The gallbladder was reported as only seen on axial T2 weighted images (Fig. 1). The impression was the patient may have chronic cholecystitis with a shrunken gallbladder. Given the experience of the hepatobiliary surgeon involved in the case, a decision was made to proceed to laparoscopic cholecystectomy.
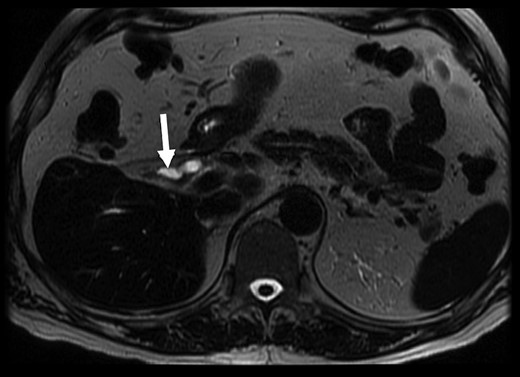
MRCP with suggestion of gallbladder adjacent to CBD (arrow). T2 weighted axial MRCP image, 3.0 T GE MRI.
On laparoscopy, the gallbladder could not be identified on exploration of the liver bed. The principle of safe dissection, above axis of the sulcus of Rouviere, was followed to identify landmarks. MRCP imaging was reviewed again intra-operatively to help guide the surgical team and avoid commencing the dissection too low, given that a gallbladder was not present in the fossa. A 2 cm cystic duct stump and cystic artery was identified (Fig. 2). An intra-operative cholangiogram was performed, confirming a distal CBD filling defect (Fig. 3). CBD clearance under direct vision with choledochoscopy was performed to extract a 7 mm stone. The cystic duct was then secured with two PDS Endoloop® Ligatures and sent for histology. A drain tube was placed along the liver bed.
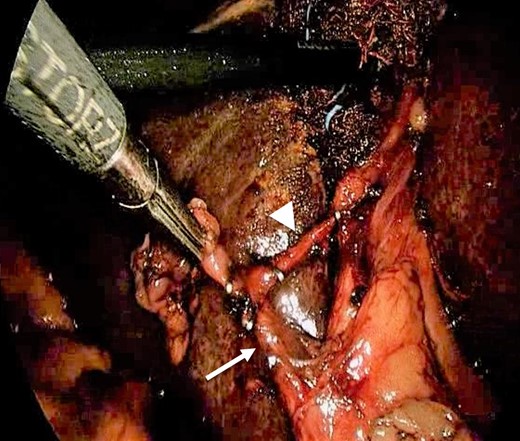
Calot’s triangle—intra-operative photograph showing cystic duct (arrow) and cystic artery (arrowhead).
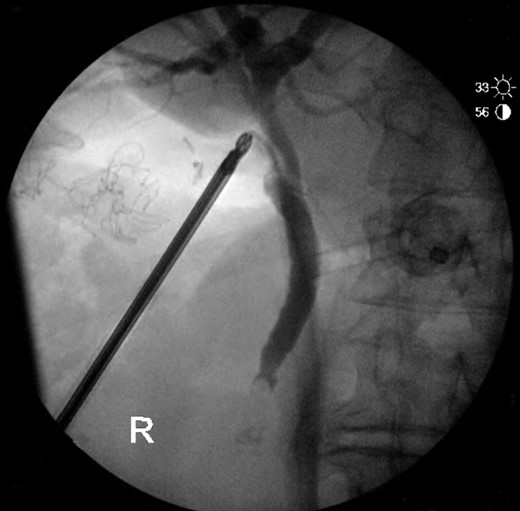
Intra-operative cholangiogram with filling defect in distal CBD.
The patient was discharged home Day 5 post-operatively following removal of his drain tube. He was reviewed in the general surgery outpatient clinic 2 weeks following discharge where he had made a good recovery. There were no symptoms or signs of post-operative complications and his pain had resolved. His bilirubin and liver function tests had returned to normal. He was subsequently discharged from clinic following this review.
DISCUSSION
It is reported that 25–50% of patients with gallbladder agenesis will develop CBD stones, suggested to be related to biliary dyskinesia [5]. Although the condition of gallbladder agenesis is rare, this is a significant rate of choledocholithiasis among this group of patients. The main treatment approach for these patients is in the form of endoscopic retrograde cholangiopancreatography (ERCP) [6]. The patient in this case was only diagnosed with gallbladder agenesis at the time of laparoscopy. In retrospect, if the surgical team had known of this diagnosis prior to this, the patient would have proceeded to ERCP. Intra-operatively, a considered decision was made to proceed following the principles of careful biliary dissection. This case demonstrates the potential for surgeons experienced in extrahepatic biliary dissection to successfully explore the CBD in a patient with gallbladder agenesis. It may be of utility in cases where an ERCP cannot be performed due to anatomical variations or prior upper gastrointestinal surgery.
Importantly, this case also highlights the difficulties in diagnosing gallbladder agenesis despite MRCP. The authors recommend a high index of suspicion in cases where the gallbladder is not definitively identified on imaging.
CONFLICT OF INTEREST STATEMENT
None declared.



