-
PDF
- Split View
-
Views
-
Cite
Cite
Boubacar Efared, Ibrahim S Sidibé, Fatimazahra Erregad, Nawal Hammas, Laila Chbani, Hinde El Fatemi, Female genital tuberculosis: a clinicopathological report of 13 cases, Journal of Surgical Case Reports, Volume 2019, Issue 3, March 2019, rjz083, https://doi.org/10.1093/jscr/rjz083
Close - Share Icon Share
Abstract
Female genital tuberculosis (FGTB) is a rare form of tuberculosis (TB) affecting women of reproductive age. The clinical presentation is often misleading. We retrospectively collected cases of female genital tuberculosis (FGTB) diagnosed from 2006 to 2016 at our pathology department. The mean age was 39.92 years (range of 18–74 years). Most patients had reproductive age, with 30.76% postmenopausal women. Seven cases (53.84%) were addressed for histopathological analysis for clinical malignant suspicion. The diagnosis was made on eight surgical specimens (61.53%). Nine patients (69.23%) had multifocal TB. The most involved genital organs were fallopian tubes (63.84%), followed by ovaries (46.15%), endometrium (38.46%) and the cervix (23.07%). The macroscopic aspects of all resected specimens did not show the classic appearance of caseous necrosis. We found that most patients with genital tuberculosis present with clinical suspicion of malignancy leading to aggressive surgical management.
INTRODUCTION
Tuberculosis (TB) is one of the most frequent endemic diseases in poorer areas of the world and still remains a major world health problem [1, 2]. Pulmonary tuberculosis (PTB) constitutes the more common clinical presentation of TB [2]. Genital tuberculosis (GTB) accounts for 15–20% of extrapulmonary TB (EPTB) [3]. The incidence of female genital tuberculosis (FGTB) is higher in developing countries; the disease usually affects the fallopian tubes and endometrium leading to infertility [4, 5]. The clinical presentation is usually indolent but may be particularly misleading as it can mimic other diseases especially malignant tumours leading to inappropriate clinical management [6, 7]. We report herein a retrospective series of 13 cases of FGTB histologically diagnosed at our pathology department.
MATERIALS AND METHOD
We retrospectively collected cases of FGTB diagnosed from 2006 to 2016, at the Department of Pathology of Hassan II University hospital, Fes, Morocco. The diagnosis of FGTB has been made by histological analysis performed on paraffin-embedded and formalin fixed tissues stained by haematoxylin-eosin (H&E). The histological diagnosis of TB was based on the evidence of lesions showing granulomas associated with typical caseous necrosis. Cases with granulomatous lesions with equivocal caseous necrosis have been excluded. Available patients’ clinical data were registered from requests forms and archival electronic files.
RESULTS (CASES)
We have registered 13 cases of FGTB, the mean age was 39.92 years (range of 18-74 years) (Table 1). Most patients had reproductive age, with only four post-menopausal women (30.76%).
Clinicopathologic characteristics of our 13 cases with female genital tuberculosis (FGTB)
| Cases . | Age (year) . | Suspicion of malignancy . | Genital site . | Extra genital site . | Specimen . | Macroscopic aspect . | Surgery . |
|---|---|---|---|---|---|---|---|
| 1 | 70 | + | Cervix, endometrium, FTs, left ovary | - | Surgical | Irregular and hard endometrium | Hystero-salpingo-oophorectomy |
| 2 | 24 | - | Ovary, FT | Peritoneum | Biopsy | - | - |
| 3 | 27 | - | Ovary, FT | - | Surgical | Distended FT, thick wall | Salpingo-oophorectomy |
| 4 | 22 | + | Cervix, endometrium | Lymph node | Surgical | Necrosis | Hystero-salpingo-oophorectomy |
| 5 | 25 | - | Endometrium | - | Biopsy | - | - |
| 6 | 28 | + | Ovary, FT | - | Surgical | Distended FT, thick wall | Salpingo-oophorectomy |
| 7 | 18 | - | FTs | Peritoneum | Surgical | Quite normal | salpingectomy |
| 8 | 62 | + | Endometrium, FTs | Lymph node | Surgical | Haemorrhage | Hystéro-salpingo-oophorectomy |
| 9 | 74 | + | Endometrium | Peritoneum | Biopsy | - | - |
| 10 | 74 | + | cervix | - | Biopsy | - | - |
| 11 | 34 | - | FTs | - | Surgical | Necrosis, haemorrhage | Salpingectomy |
| 12 | 23 | + | Ovaries | Peritoneum | Surgical | Cystic change, haemorrhage | Oophorectomy |
| 13 | 38 | - | Ovary | Peritoneum | Biopsy | - | - |
| Cases . | Age (year) . | Suspicion of malignancy . | Genital site . | Extra genital site . | Specimen . | Macroscopic aspect . | Surgery . |
|---|---|---|---|---|---|---|---|
| 1 | 70 | + | Cervix, endometrium, FTs, left ovary | - | Surgical | Irregular and hard endometrium | Hystero-salpingo-oophorectomy |
| 2 | 24 | - | Ovary, FT | Peritoneum | Biopsy | - | - |
| 3 | 27 | - | Ovary, FT | - | Surgical | Distended FT, thick wall | Salpingo-oophorectomy |
| 4 | 22 | + | Cervix, endometrium | Lymph node | Surgical | Necrosis | Hystero-salpingo-oophorectomy |
| 5 | 25 | - | Endometrium | - | Biopsy | - | - |
| 6 | 28 | + | Ovary, FT | - | Surgical | Distended FT, thick wall | Salpingo-oophorectomy |
| 7 | 18 | - | FTs | Peritoneum | Surgical | Quite normal | salpingectomy |
| 8 | 62 | + | Endometrium, FTs | Lymph node | Surgical | Haemorrhage | Hystéro-salpingo-oophorectomy |
| 9 | 74 | + | Endometrium | Peritoneum | Biopsy | - | - |
| 10 | 74 | + | cervix | - | Biopsy | - | - |
| 11 | 34 | - | FTs | - | Surgical | Necrosis, haemorrhage | Salpingectomy |
| 12 | 23 | + | Ovaries | Peritoneum | Surgical | Cystic change, haemorrhage | Oophorectomy |
| 13 | 38 | - | Ovary | Peritoneum | Biopsy | - | - |
FT: fallopian tube; FTs: Fallopian tubes; +: suspicion of malignancy; -: no suspicion of malignancy.
Clinicopathologic characteristics of our 13 cases with female genital tuberculosis (FGTB)
| Cases . | Age (year) . | Suspicion of malignancy . | Genital site . | Extra genital site . | Specimen . | Macroscopic aspect . | Surgery . |
|---|---|---|---|---|---|---|---|
| 1 | 70 | + | Cervix, endometrium, FTs, left ovary | - | Surgical | Irregular and hard endometrium | Hystero-salpingo-oophorectomy |
| 2 | 24 | - | Ovary, FT | Peritoneum | Biopsy | - | - |
| 3 | 27 | - | Ovary, FT | - | Surgical | Distended FT, thick wall | Salpingo-oophorectomy |
| 4 | 22 | + | Cervix, endometrium | Lymph node | Surgical | Necrosis | Hystero-salpingo-oophorectomy |
| 5 | 25 | - | Endometrium | - | Biopsy | - | - |
| 6 | 28 | + | Ovary, FT | - | Surgical | Distended FT, thick wall | Salpingo-oophorectomy |
| 7 | 18 | - | FTs | Peritoneum | Surgical | Quite normal | salpingectomy |
| 8 | 62 | + | Endometrium, FTs | Lymph node | Surgical | Haemorrhage | Hystéro-salpingo-oophorectomy |
| 9 | 74 | + | Endometrium | Peritoneum | Biopsy | - | - |
| 10 | 74 | + | cervix | - | Biopsy | - | - |
| 11 | 34 | - | FTs | - | Surgical | Necrosis, haemorrhage | Salpingectomy |
| 12 | 23 | + | Ovaries | Peritoneum | Surgical | Cystic change, haemorrhage | Oophorectomy |
| 13 | 38 | - | Ovary | Peritoneum | Biopsy | - | - |
| Cases . | Age (year) . | Suspicion of malignancy . | Genital site . | Extra genital site . | Specimen . | Macroscopic aspect . | Surgery . |
|---|---|---|---|---|---|---|---|
| 1 | 70 | + | Cervix, endometrium, FTs, left ovary | - | Surgical | Irregular and hard endometrium | Hystero-salpingo-oophorectomy |
| 2 | 24 | - | Ovary, FT | Peritoneum | Biopsy | - | - |
| 3 | 27 | - | Ovary, FT | - | Surgical | Distended FT, thick wall | Salpingo-oophorectomy |
| 4 | 22 | + | Cervix, endometrium | Lymph node | Surgical | Necrosis | Hystero-salpingo-oophorectomy |
| 5 | 25 | - | Endometrium | - | Biopsy | - | - |
| 6 | 28 | + | Ovary, FT | - | Surgical | Distended FT, thick wall | Salpingo-oophorectomy |
| 7 | 18 | - | FTs | Peritoneum | Surgical | Quite normal | salpingectomy |
| 8 | 62 | + | Endometrium, FTs | Lymph node | Surgical | Haemorrhage | Hystéro-salpingo-oophorectomy |
| 9 | 74 | + | Endometrium | Peritoneum | Biopsy | - | - |
| 10 | 74 | + | cervix | - | Biopsy | - | - |
| 11 | 34 | - | FTs | - | Surgical | Necrosis, haemorrhage | Salpingectomy |
| 12 | 23 | + | Ovaries | Peritoneum | Surgical | Cystic change, haemorrhage | Oophorectomy |
| 13 | 38 | - | Ovary | Peritoneum | Biopsy | - | - |
FT: fallopian tube; FTs: Fallopian tubes; +: suspicion of malignancy; -: no suspicion of malignancy.
A substantial proportion of women’s specimens were addressed for histopathological analysis for malignant suspicion on clinical examination and on imaging techniques (seven cases, 53.84%). These patients presented with abnormal bleeding (especially metrorrhagia in older patients) or with mass-forming lesions on clinical examination and on imaging techniques. Diverse surgical procedures were performed on eight cases (61.53%). Most patients had multifocal FGTB (9 cases, 69.23%) with extragenital involvement especially peritoneal or lymph node locations (five and two cases respectively). The most involved genital organs (whether solely or with other organs) were fallopian tubes (63.84%), ovaries (46.15%), endometrium (38.46%) and the cervix (23.07%). The patient No-8 had a concomitant cervical adenocarcinoma. The macroscopic aspects of all resected specimens did not show the classic cheese-like appearance of the caseous necrosis (Fig. 1), rather they show morphologic abnormalities (distended fallopian tubes, hard endometrium), haemorrhage, cystic changes or ischaemic necrosis. The histopathological analysis showed granulomatous lesions associated with variable amount of caseous necrosis (Figs 2 and 3). All patients were HIV-negative, they received the standard antibiotic therapy (combination of rifampicin, isoniazid, ethambutol and pyrazinamide).

Macroscopic view: an illustrative case of lymph node tuberculosis with cheese-like appearance of the caseous necrosis (arrow).
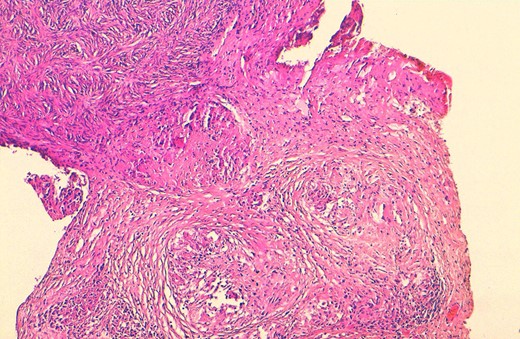
Histological view showing ovarian parenchyma with granulomatous lesions and caseous necrosis (H&E × 100).
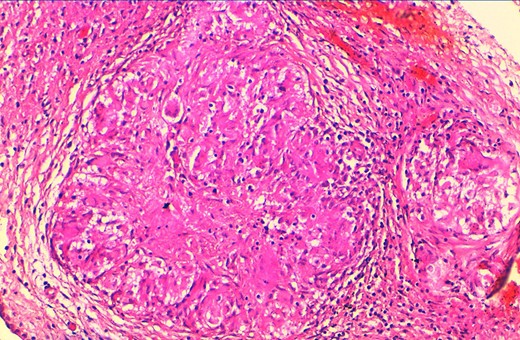
At higher magnification, tuberculosis granulomas include epithelioid and giant cells, plasma cells and caseous necrosis, along with fibrotic changes (H&E × 200).
DISCUSSION
The current study reports cases of FGTB diagnosed at the Department of Pathology of Hassan II university hospital of Fes, Morocco, an endemic country where the incidence of TB in 2008 was 81 per 100,000 overall, with 28 000 new cases each year [8, 9]. Typically, the incidence of FGTB is higher in developing countries, around 5–21% [3]. The disease affects mostly women of reproductive age. Our study recapitulates this epidemiologic feature as the mean age was 39.92 years with 30.76% of postmenopausal women. In fact, the atrophic endometrium of older women is not a favourable milieu for the development of Mycobacterium tuberculosis, and this feature could explain why TB is rare in postmenopausal patients as well as in other organs like the breast or the spleen [1, 10].
Usually FGTB is as an indolent disease, rarely patients present with abdominal pain, abnormal genital bleeding, dyspareunia [1]. Sometimes patients with FGTB present with a misleading clinical and radiological symptoms such as ascites or abdominal distension, leading to suspicion of malignant tumours especially in older patients [6, 7]. Also, FGTB is sometimes an incidental finding during investigations of women with infertility [4]. The upper genital tract (fallopian tubes and the endometrium) is mostly affected in FGTB [2, 5]. In the current series, we found that fallopian tubes were more frequently involved (63.84%), followed by the ovaries (46.15%) and the endometrium (38.46%). However some studies reported highest involvement of the endometrium [2].
The diagnosis of FGTB relies on several diagnostic tools. As the disease is usually silent with non-specific and misleading signs, the diagnosis can be challenging. Patients with tubo-ovarian TB associated with peritoneal involvement (ascites) and a frequent associated high level serum CA-125, are often misdiagnosed as ovarian carcinoma and undergo unnecessary and aggressive surgery [6, 7]. In our study, a substantial proportion of cases have been addressed for suspicion of malignant tumours (seven patients, 53.84%). Imaging techniques are useful in the diagnosis of FGTB but not specific. The acid fast stain (Ziehl-Neelsen stain) or Mycobacterium tuberculosis culture require adequate sampling with bacillary lesions, unfortunately FGTB lesions are usually pauci-bacillary [1]. The molecular diagnosis by polymerase chain reaction (PCR) has a good sensitivity but not affordable in poor areas where TB is endemic [10]. The histopathological analysis is a very useful diagnostic tool as FGTB are usually paucibacillary. This diagnostic tool also plays a major role in ruling out malignant tumours. The histological lesions of TB show granulomas with multinucleated giant cells, epithelioid cells associated with caseous necrosis [2]. However these features are not present in the early beginning of the TB. The histopathological analysis also requires adequate sampling especially during laparascopic evaluation. In fact, the diagnosis of FGTB is challenging as laparoscopy can be very dangerous because there might be many adhesions involving omentum and bowels. In such circumstances, open laparoscopy remains the more adequate and safer technique. However, FGTB presents rarely with macroscopic caseous necrosis, hence the necessity of careful macroscopic sampling. In our series, none of the resected specimens presented macroscopic aspect of caseous necrosis.
CONCLUSION
In summary, FGTB is a form of EPTB affecting women at a reproductive age. The clinical presentation is sometimes misleading as it suggests a malignant tumour. The histopathological analysis provides the correct diagnosis and rules out the diagnosis of malignancy.
CONFLICT OF INTEREST STATEMENT
All authors declare that they have no competing interest.
FUNDING
The authors received no specific funding for this study.



