-
PDF
- Split View
-
Views
-
Cite
Cite
Raguraj Chandradevan, Ian H Rutkofsky, Mary Charmaine E Campana, Harkirat Kaur, Felisha L Kitchen, Craig C Odum, Randolph S Devereaux, James D Colquitt, Sarah E Hamler, John T Williams IV, A diagnostic dilemma of appendicular mass in an elderly patient: a case report and literature review, Journal of Surgical Case Reports, Volume 2019, Issue 3, March 2019, rjz059, https://doi.org/10.1093/jscr/rjz059
Close - Share Icon Share
Abstract
Primary appendicular adenocarcinoma is a rare tumor, mucinous variety, being most common. The case presentation highlights the unusual appearance and diagnostic dilemma of an appendicular adenocarcinoma. Our elderly patient presented with an ill-defined tender lump which later was diagnosed as a perforated appendicular adenocarcinoma, responsive to single-staged surgery and adjunct chemotherapy. We considered the single-staged surgery since the appendix was perforated and right colectomy would not aid the prognosis. High index of clinical suspicion for malignancy should be kept in mind for elderly patients presenting with an appendicular lump. Every effort should be made during the elective surgery to remove the mass during the single-staged surgery.
INTRODUCTION
Appendicular adenocarcinoma is a rare entity often presenting as a post-operative diagnosis by the pathologist. Cancers of the appendix have a variety of presentations, often like acute appendicitis, a palpable mass in the right iliac fossa or a rupture of the appendix [1]. In one series of studies, the age-adjusted incidence of appendicular cancer is recorded as 0.12 cases per 1,000,000 people/year [2]. The most common histopathological tumor types of appendicular masses are carcinoid and adenocarcinoma. Benign histopathology include leiomyomas, lipomas and angiomas [3]. An elderly patient presented as a phlegmonous mass, which was treated conservatively, later on, presented as a reproduction of symptoms. After resection of the mass with appendectomy and partial cecectomy, histopathology of the mass was suggestive of mucinous adenocarcinoma. The patient was followed up with chemotherapy as per the special circumstance.
CASE REPORT
An 81-year-old morbidly obese female with the past medical history of Type-II diabetes mellitus and uncontrolled hypertension presented to the Emergency department with right lower quadrant abdominal pain. The pain was throbbing in nature, 10/10 in severity, and constant, lasting for few hours at a time, and exacerbated with movement. Further questioning revealed she had ongoing abdominal pain for a week. The pain aggravated with the movements and relieved by pain medications and rest. She also had associated weight loss of 7–8 pounds within 3 months and also complains of nausea and episodes of vomiting for the last 3 weeks. She did not have any change in bowel habits or change in dietary habits. There was no associated history of fever or bladder habits.
The patient had a previous admission 4 weeks back with the same kind of complaint, but according to the patient, went for an outpatient follow-up upon with her OB/GYN doctor. Upon presentation with at the outpatient department, with the wage ongoing right-sided discomfort for few weeks, the physician placed an order for a computerized tomography (CT) scan which identified a mass-like density in the base of the cecum with extra luminal soft tissue thickening and probable developing phlegmon (Fig. 1) not yet percutaneously drainable measuring (47 × 37 mm). She was advised to go to the emergency department. During the admission, she spent 5 days in the hospital as an inpatient and was treated for a phlegmonous abscess of the appendix, as per the CT indicated. During the hospital course, she was treated with Flagyl 500 mg IV TID and Aztronam 1 g TID for 5 days and, during discharge, she was given PO Flagyl Q8H and PO Bactrim Q12 H for another 9 days. She was advised to follow-up with the surgical outpatient services to schedule an interval appendectomy with the resolution of the inflammation. She soon developed a recurrent episode of abdominal pain, starting 3 weeks post-discharge and was re-admitted with worsening reproduction of the prior symptoms.
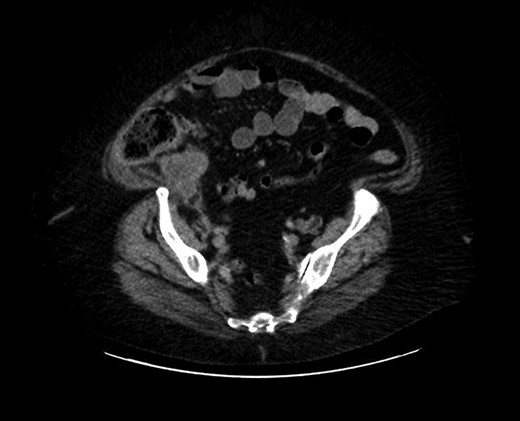
Cross section of abdominal computed tomography showed an appendiceal tumor.
During the readmission, the patient was non-febrile, vital signs were within normal limits and system examination was normal except for abdominal. Abdominal examination revealed an ill-defined tender lump in the right iliac fossa with no guarding, rigidity or re-bound tenderness. Rectal examination was unremarkable. Investigations revealed a white blood cell (WBC) count of 10,000/mm3. ESR and CRP were within normal limits. Further investigations were normal. In view of the patient’s presentation, history, examination and laboratory findings, the possibility of appendicular abscess, carcinoid tumor, adenocarcinoma, mucinous cystadenocarcinoma and ileocecal Koch’s was considered.
CT scan of the abdomen revealed stable soft tissue focus and adjacent rim of enhancing low-density collection along the posteromedial and posterior aspects of the cecum in the right lower abdomen (Fig. 2). Suggestive of the possibility of chronic infectious or neoplastic etiologies of appendicular origin. The appendix was not visualized as a separate structure. Comparison of the previous CT excluded worsening of the intra-abdominal or intra-pelvic process. Upon discussion with medical and surgical teams, reproduction of symptoms and CT evidence, aided the direction for surgical intervention. On the second day of hospital admission, surgical laparoscopy located the terminal ileum with adhesions from the sidewall. The findings included perforated viscus and mass at the appendicular base. With this appearance, a direct intervention was impossible, we proceeded with hand-assisted partial cecectomy, appendectomy and removed the entire mass.
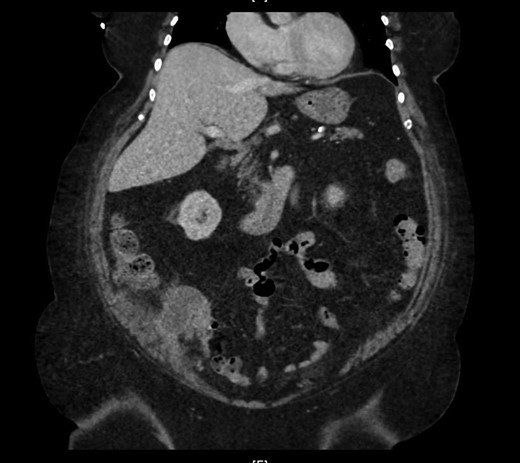
Marked appendiceal wall swelling and intraluminal filling defect of contrast medium over appendix noted in the coronal CT-image.
SURGICAL TECHNIQUE
The patient was administered general anesthesia with placement of endotracheal tube. Our patient was prepped with betadine for a vaginal/perineal prep and chloroprep was used on the abdomen. After sterile draping of the patient, and official time-out with all in agreeance, General Surgeon scrubbed in and proceeded with the insertion of veress needle and insufflated the abdominal cavity with CO2. Once the abdominal pressure reached 12 mmHg, the general surgeon then placed a hand port in the lower midline. Placement of hand in to break-up any adhesions from the sidewall as it felt like it had been perforated by a large mass at the appendicular base. We were able to locate the terminal ileum, used the LigaSure™ device to divide the mesentery and lateral attachments and then took a GIA stapler and divided the cecum. The mass was then grasped and brought out through the hand port. There was a wound protector in the hand port. We then irrigated and lavage the area, sucking all the free fluid out of the abdomen, then, we removed the hand-assist device, make sure the area was hemostatic and then we closed with PDS suture and skin staples.
The cecum measures 8 × 6 cm and appendix is dilated and measures 7 cm × 2 cm. The mucosa at the appendicular orifice demonstrates a polypoid appearing mass measuring 3.2 × 1.5 cm (Fig. 3). Grossly the mass extends throughout the appendix and measures approximately 7.7 cm × 2 cm. The distal aspect was hemorrhagic and ragged, with an opened ragged defect measuring 1 cm in greatest dimension (Fig. 4). The majority of the appendicular serosa was tan and smooth, with scattered red areas. Grossly, the tumor is 1.5 cm from the mesenteric margin. Multiple lymph node candidates are identified. One lymph node candidate measures up to 5 mm and is 4 mm from the mesenteric margin.


A longitudinal cross section of the appendix, adenoma at appendiceal orifice on left, hemorrhagic tip rupture on right.
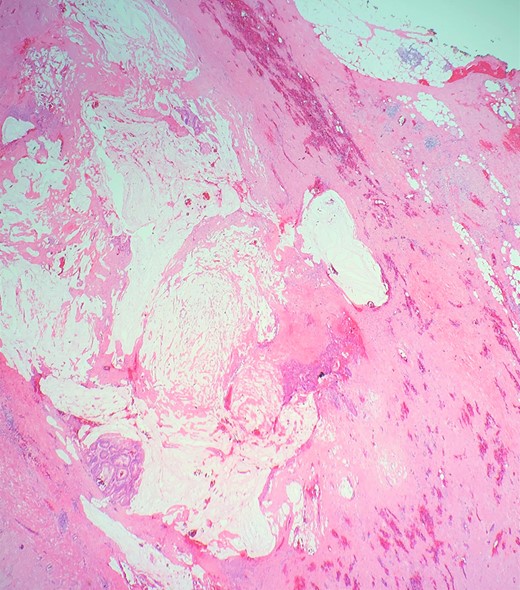
Definitive histological examination showed perforated appendix involved by moderately differentiated mucinous adenocarcinoma (Fig. 5), arising in the background of diffuse tubulovillous adenoma with extensive high-grade dysplasia and showed cellular mucin within the periappendiceal soft tissue (Figs 6 and 7). Proximal cecal mucosal margin and mesenteric margin uninvolved by carcinoma and four periappendicular lymph node was negative for metastatic carcinoma and pathological stage aided for pT4a, pN0. The post-operative course was uneventful. The tumor was staged as T4N0M0 (Modified Astler Coller B3). Patient was referred for oncology and for multidrug adjuvant chemotherapy of 5-fluorouracil, lecovorin and oxalipatin (FOLFOX) was given. Patient was asymptomatic during the 2 weeks, 3 months and 6 months follow up.
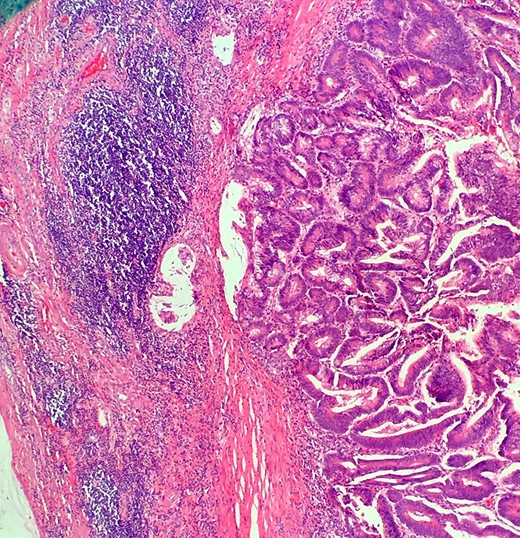
This demonstrates mucinous tumor with pushing invasion through the appendiceal wall.
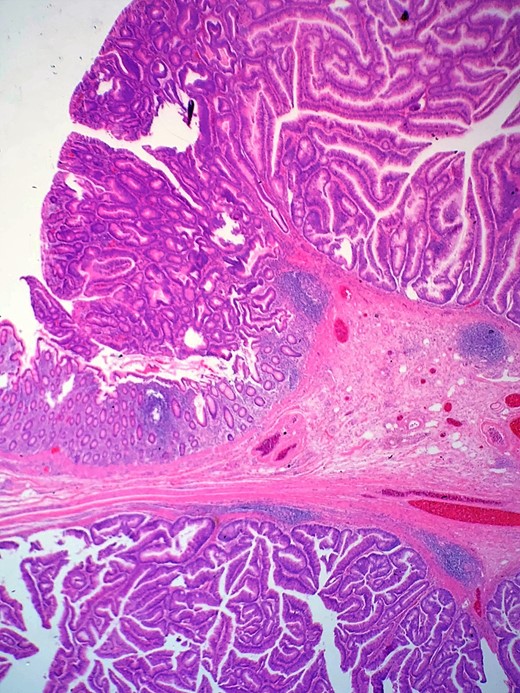
Shows transition of normal cecal mucosa to high-grade tubulovillous adenoma at the appendiceal orifice.
DISCUSSION
The international classification of disease for oncology divides tumors of appendix into malignant carcinoid, goblet cell carcinoma, colonic type adenocarcinoma, mucinous adenocarcinoma and signent-ring cell carcinoma [4]. Of all the variants, mucinous types are well differentiated and slow growing, this variant has the best prognostic factor [5]. Appendicular malignancies represent less than 0.5% of all gastrointestinal tumors [2]. Because adenocarcinoma of the appendix is so rare, its clinical presentation and natural history are still not well described or understood. Most often the clinical presentation is acute appendicitis or an abdominal mass, as were the findings seen in our patient, but preoperative diagnosis is rarely evident and most patients are not identified until the advancement of the disease [6].
Adenocarcinoma of the appendix spread via local invasion, lymphatic vessels and blood stream. The anatomic structure of the appendix allows several contributions in regard to appendicular neoplasms to be made. The narrow and confined diameter predisposes to occlusion of the lumen by the neoplasm early in its disease course. This creates the potential for superimposed appendicitis and marked possibility to rupture and appendicular carcinoma associated with perforation [7]. This potentially aides for early peritoneal dissemination. Likewise in the presentation of our elderly patient, the mass was occupying the appendix and as well as part of the cecum and, during histology examination, it revealed that the appendix is perforated and there is a high possibility of peritoneal seeding.
The simple appendectomy seemed to be sufficient for pT1 carcinoma of the appendix, most tumors present as advanced invasive carcinoma and secondary radical hemicolectomy is usually recommended as the operative treatment of choice [8]. Malignant infiltration of local regional lymph nodes is expected in about one-third of the patients especially in advanced invasive tumors, adjuvant chemotherapy is recommended [9]. The prognostic factors in primary adenocarcinoma of appendix depend upon tumor stage, histology, grade, size and the type of surgery [6]. Even though the survival was better in patients undergoing right radical hemicolectomy [1], we restricted the surgery to the appendix and cecum with the mass as a single-staged procedure. We considered the patient’s age and comorbidities especially obesity, the gross/histology findings of perforated appendix and after a multidisciplinary in-hospital team meeting between surgeons, oncologist hospitalist and the patient and family members. The patient and her family agreed with the care of management. Ultimately, the patient received adjunct chemotherapy.
CONCLUSION
The emphasis of the case report highlights the difficulty in the preoperative diagnosis of appendicular carcinoma in patients presenting with an appendicular mass. This shows that the expectant management of the patient with appendicular carcinoma is multifactorial. We also emphasize that in elderly patients presenting with appendicular mass, the differential diagnosis of malignancy should be considered. Keeping this diagnosis and better adherence to oncological principles during the single-staged procedure would save patients from dissemination of malignancy and provide the better prognosis.
CONFLICT OF INTEREST STATEMENT
None declared.



