-
PDF
- Split View
-
Views
-
Cite
Cite
David Aguirre-Mar, Berta A Serrano, Carlos Morales, Katerina Toro, Julian Burgos, Long-term success of complex recurrent rectovaginal fistula repair, Journal of Surgical Case Reports, Volume 2019, Issue 3, March 2019, rjz001, https://doi.org/10.1093/jscr/rjz001
Close - Share Icon Share
Abstract
Rectovaginal fistulas (RVF) are the cause of major affliction to the affected patient and are a foremost challenge for the attending surgeon. Traditional techniques for treatment of RVF are quite extensive and particularly invasive. A more local procedure, with an acceptable success rate, would be the ideal first approach in treatment of this particular ailment. The aim of the current study is to show the step-by-step technique to correct a complex recurrent RVF (rRVF) using a biomesh implant. A 61-year-old female, who had undergone a prior vaginal hysterectomy, presented with a complex recurrent RVF. A third attempt to repair the RVF was conducted by a surgical team with the utilization of a biomesh, which resulted in no further recurrence of symptoms or RVF for up to 4 years. Complex rRVF repair by the placement of the biomesh allows for a secure and sustainable closure with potentially better prognosis for the patients.
INTRODUCTION
A rectovaginal fistula (RVF) is a disconcerting condition that is not easily remediated. The symptoms include the passage of gas and fecal matter through the vagina, vaginal inflammation and/or recurrent vaginal infections, and dyspareunia. RVF present with very negative influences on the quality of life of patients [1]. The most common cause of an RVF is obstetrically related and often due to trauma caused during childbirth. Other common causes of RVF are known to be Crohn’s disease, surgical trauma, infection disease, neoplasia and radiation [2]. Different surgical techniques for reparation of an RVF are as follows: advanced endorectal flaps, with a success rate of 85%, which diminishes to 55% with two or more reparations, gracilis muscle transposition, with a success rate of 47–85%, Martius flap (bulbocavernosus muscle), and the transposition of tissue such as the omentum, anterior rectus muscle, and/or fat tissue; many of these accomplished through a laparoscopic approach [3]. If the application of the specific Biodesign mesh, previously mentioned, were to be utilized in the repair of complex recurrent RVF, then we would expect to observe a potentially higher rate of long-term fistula closure, a better longstanding prognosis, as well as a lower rate of morbidity for patients undergoing this surgical procedure.
CASE REPORT
We present the case of a 61-year-old Latin-Caucasian female patient with no previous familial hereditary conditions; social history of heavy tobacco consumption and surgical history of an Abdominoplasty. Her past OBGyn history includes vaginal hysterectomy (VH) in other Hospital with unknown diagnosis, 2 years prior to our admission. Four days post-VH the patient experienced passage of gas through the vagina, urinary incontinence and nocturia; later, she experienced vaginal passage of fecal matter. Two weeks after the VH, first intent to fistula repair through vagina by OBGyn Service was performed.
One month later, recurrence of the fistula tract and symptoms resulted in our surgical consultation. A second repair using transanal mucosal/submucosal flap and fibrin sealant was completed at my service, closing the rectal wall defect. Two months later, a third recurrence of symptoms and fistula occurred, with severe sexual life and QoL dissatisfaction. New examination confirmed the diagnosis. Evident fibrosis, 5 cm from the anterior anal verge, was also observed. All Lab workup was normal.
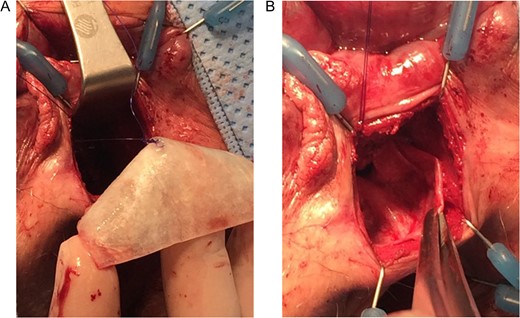
Prior to our surgical intervention, a rigid anoscopy and a flexible colonoscopy were performed, confirming recurrent RVF. Differential diagnosis such as IBD (UC/Crohn’s), chronic infection and local foreign body reaction were ruled out in this patient. Exploratory surgery under anesthesia was conducted and presence of a RVF was found, with an orifice at the 5 cm mark from the anal verge and loss of mucosa and submucosa of 1 cm at the anteromedial line, was observed (Fig. 1). A 1 cm orifice was observed at the vaginal surface corresponding to rectal side of the fistula orifice (Fig. 1).
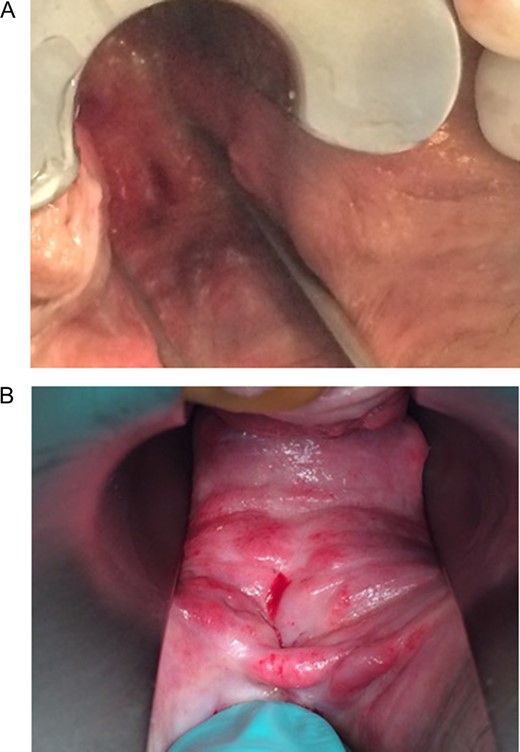
(A and B) A rectovaginal fistula orifice located 5 cm from the anal border. (A)View from the rectum. (B) View from the vagina.
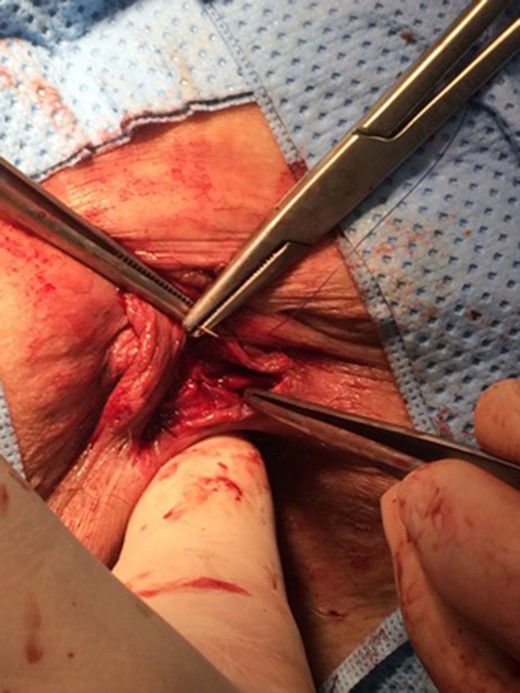
In a lithotomy position, resection of fibrous tissue and fistula orifice at the vaginal surface was accomplished (Fig. 2). A transverse perineal incision was then performed in order to divide the rectovaginal septum (RVS) (Figs 3 and 4). The vagina was then thoroughly and attentively separated from the sphincter, anal wall and rectal wall up to a 6 cm mark inward.
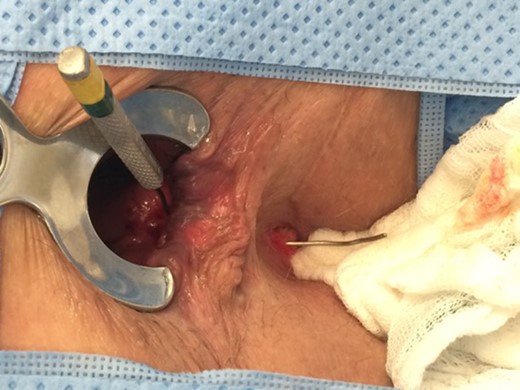
Image showing the compartment communication via the fistula tract.

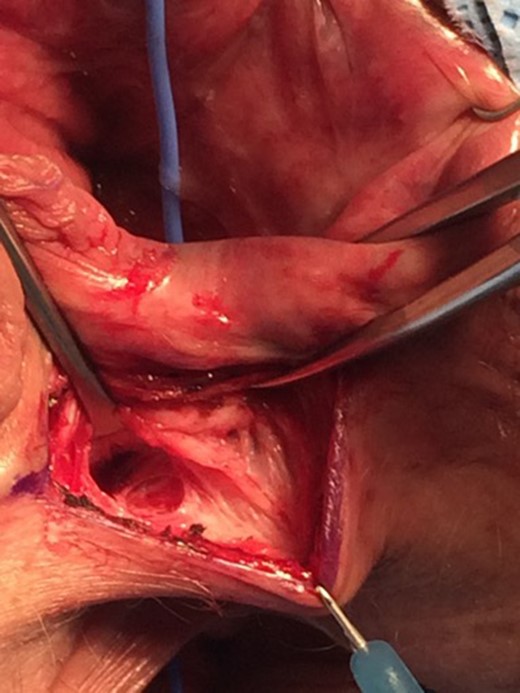
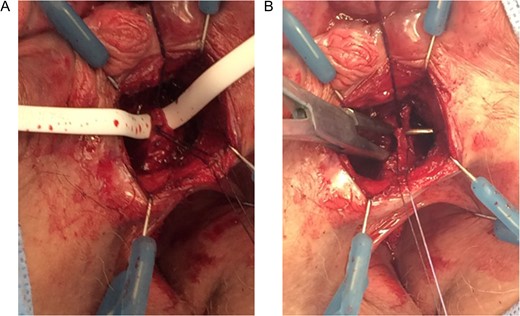
In order to accurately perform the resection and ligation of fistula tract, the tract was first identified (Fig. 5) and then ligated with total PDS4-0/4-0Vicryl ligatures. Then biomesh (biological bovine small intestine mesh) was placed and fixed between the rectal and vaginal wall (RVS) with suture and fibrin sealant (Fig. 6). At the rectal wall, a new advancement flap covered the anal side of previous fistula area.
(A and B) Marking of the fistula tract. (A) Penrose drainage used to identify fistula tract. (B) Lift procedure view.
(A and B) Placement of the Biomesh at the rectovaginal septum with sutures and fibrin sealant.
DISCUSSION
The reparation techniques of RVFs known as tissue and muscle flap transpositions are based on the necessity to move and place live vascularized tissue at the RVS. Here we describe a technique in which a biomesh is used without the need of any crosslinks, which permits the development of new tissue within the mesh itself and is highly resistant to infection (Fig. 7).
More invasive techniques, such as the use of flaps or vascularized tissue transposition, present with good fistula closure rates (50–100%), but none have been previously analyzed as part of a randomized controlled study [4, 5]. Those techniques are linked to high morbidity rates, as well as a decline in the quality of life of the patient, such as a diminished or nonexistent sexual function [6].
The first publication related to the treatment of RVF using mesh, was done by Moore et al. [7]. Afterwards the placement of a mucosal mesh obtained from the bovine small intestine was described [8, 9]. In this patient the 4 years follow up period add positive long-term result experienced by the patient. This biomesh presented a success rate between 71 and 81.5%, and the duration of follow up was between 12 and 22 months. A more recent study published by Göttgens et al. [10], with a success rate of 75%, determined that prior radiation in patients was a critical and important negative factor in the successful closure of any RVF. The use of mesh was seen controversial in the beginning due to potentially risk of foreign body local reaction/infection. New types of meshes could potentially add extra-strength, shorten post-op times but with absorbable properties. At the same time could potentially reduce rRVF rate.
The main intention of this case is to present step-by-step detailed technique of the procedure. It is imperative to know that surgical approach taken in patients suffering from complex rRVF should be individualized to each patient at hand. We believe implementation of the biomesh could add value to some recurrent fistulas situations. If a randomize trials can be performed in a larger population, could evidence as good results as this 4 years follow up patient, potentially allowing for a step towards the standardization of the technique used in this specific ailment.
CONFLICT OF INTEREST STATEMENT
None.



