-
PDF
- Split View
-
Views
-
Cite
Cite
Manabu Yasuda, Toshihiro Osaki, Yukiko Fukuich, Kenichi Kobayashi, Teruo Iwata, Tomoko So, Anterior mediastinal tumor as a solitary lymph node metastasis of occult thyroid carcinoma, Journal of Surgical Case Reports, Volume 2019, Issue 2, February 2019, rjz029, https://doi.org/10.1093/jscr/rjz029
Close - Share Icon Share
Abstract
Solitary metastasis of occult thyroid carcinoma to the anterior mediastinum is very rare. A 65-year-old woman was examined for anterior mediastinal tumor based on the FDG accumulation on PET. We resected the tumor by video-assisted thoracic surgery. A pathological examination revealed that the tumor was lymph node metastasis of papillary thyroid carcinoma. The postoperative examination showed that the tumor was a solitary lymph node metastasis of occult thyroid carcinoma. Primary thyroid carcinoma has not appeared in 2 years since the surgery, and careful follow-up has been continued.
INTRODUCTION
Occult thyroid carcinoma had often been reported in cervical lymphadenopathy [1]. However, solitary metastasis of occult thyroid carcinoma to the anterior mediastinum is very rare in the English literature [2].
Positron-emission tomography (PET) has been established as a powerful tool for the diagnosis, clinical staging, and outcome of intrathoracic malignancies, such as lung cancer [3]. Recently, the utility of PET assessment has been reported for the evaluation of malignant behavior in thymic epithelial tumors [4].
In the present case, anterior mediastinal tumor detected based on the fluorodeoxyglucose (FDG) accumulation on PET was resected by video-assisted thoracic surgery, and the tumor was diagnosed as occult thyroid carcinoma.
CASE REPORT
An asymptomatic 65-year-old woman visited our department for anterior mediastinal tumor during the follow-up period for postoperative uterine and tongue cancer. The FDG uptake on PET scans showed upregulation gradually throughout the postoperative period, with a maximum standardized uptake value (SUVmax) of 6.8 in the tumor (Fig. 1) and no accumulation at other sites. The preoperative diagnosis of the mediastinal tumor was thymoma, thymic carcinoma and metastatic tumor from uterine and tongue cancer. We performed tumor extirpation via video-assisted thoracic surgery (Video 1). A microscopic examination of the resected tumor revealed the infiltration of lymphocytes and cube-shaped tumor cells with relatively ground glass nuclei and nuclear grooves (Fig. 2). The tumor also showed positive staining for thyroid transcription factor (TTF)-1, and the histopathological diagnosis was lymph node metastasis of papillary thyroid carcinoma.
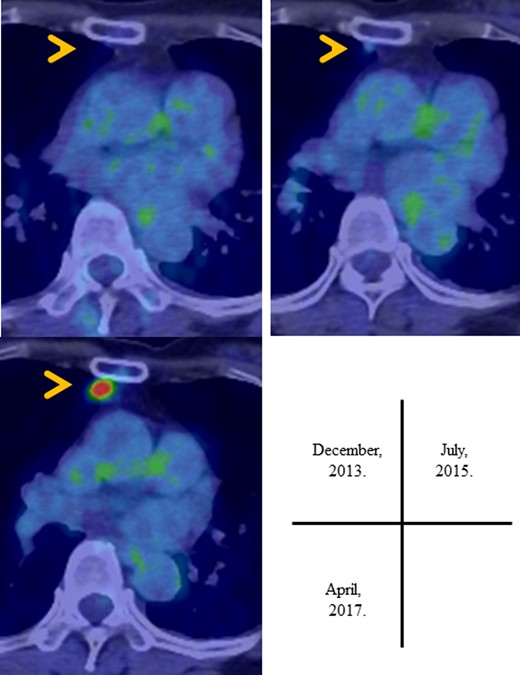
PET scan showed in the accumulation of FDG in the anterior mediastinal tumor in the follow-up period.
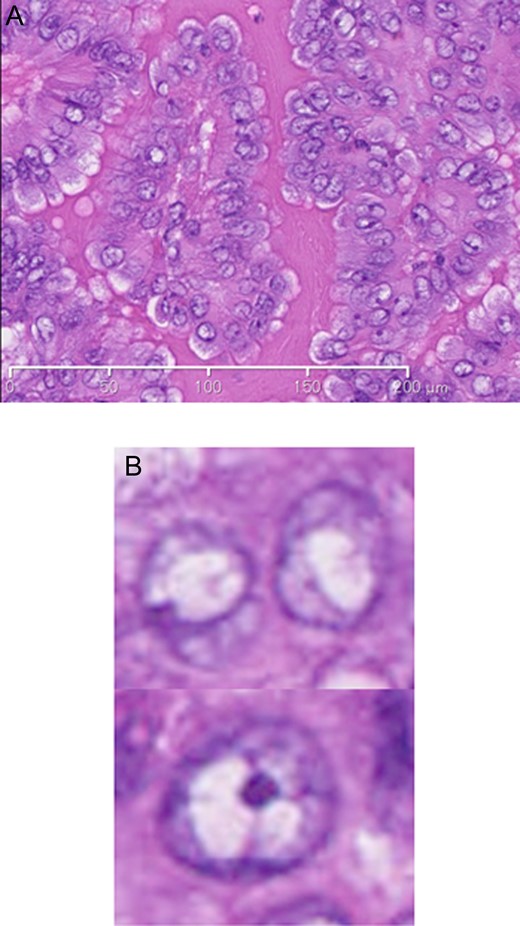
The pathological findings of specimens from the tumor: (A) A microscopic examination of the resected tumor revealed papillary carcinoma (B) and tumor cells with relatively ground glass nuclei and nuclear grooves (hematoxylin and eosin staining).
Based on the pathological findings and results of a postoperative examination, the anterior mediastinal tumor was deemed a solitary lymph node metastasis of occult thyroid carcinoma. We consulted endocrinologists and thyroid surgeons, and confirmed postoperative follow-up plan for the patient without thyroidectomy. The postoperative recovery was favorable, and the patient has been well without appearance of primary thyroid carcinoma in 2 years since the surgery.
DISCUSSION
In this case report, we describe a rare case of occult thyroid carcinoma diagnosed as a metastasis to the anterior mediastinum. Occult carcinoma is a primary microcarcinoma in which metastatic lesions are detected first. The incidence of occult thyroid carcinoma in thyroid carcinoma is 0.1–2.2% [5]. Thyroidectomy is often performed for primary microcarcinoma in occult thyroid carcinoma. Marchesi et al. [6] reported that 26 out of 38 cases (68%) of thyroid microcarcinoma had laterocervical lymph node metastasis. Bilimoria et al. [7] also reported that the ideal treatment for patients with tumors <1 cm in size was thyroid lobectomy based on an analysis of 40 000 patients. However, surgery may not be the optimum treatment approach for papillary microcarcinoma. Ito et al. [8] found that only 6.7% of low-risk patients with papillary microcarcinoma had an increased lesion size at 5 years’ follow-up. Furthermore, none developed additional distant metastasis or died of thyroid carcinoma. Our patient has been well without the appearance of primary thyroid carcinoma in 2 years since her surgery. On the other hand, it was reported that primary carcinoma appeared 4 years after resection of the metastatic tumor [1]. Whether or not occult thyroid carcinoma should be treated with thyroidectomy is controversial, and the further accumulation of experience on occult thyroid carcinoma is required.
Recently, the utility of PET assessments for the evaluation of malignant behavior in thymic epithelial tumors has been reported [3, 4]. In thyroid carcinoma, the utility of PET is limited in the diagnosis and postoperative follow-up. Among less-differentiated thyroid carcinoma, such as medullary carcinoma and undifferentiated carcinoma, PET has emerged as a valuable tool, because of the enhanced glucose metabolism. However, well-differentiated lesions such as papillary thyroid carcinoma do not always show the accumulation of FDG. In general, PET is known to be useful in the follow-up of differentiated thyroid carcinoma patients with elevated serum thyroglobulin levels and negative radioiodine whole-body scans [9]. However, the FDG avidity of differentiated thyroid carcinoma has been shown to be associated with the tumor size, lymph node metastasis, extrathyroidal extension and lymphovascular invasion, and these factors are known to be associated with a poor prognosis [10]. In our case, careful follow-up has been needed, as the FDG accumulation was recognized in the tumor. Although ultrasonography is a gold-standard tool both in the diagnosis and follow-up of thyroid carcinoma, PET was also useful for the detection of distant metastasis in papillary thyroid carcinoma, such as in our case.
CONCLUSION
We report a rare case of occult thyroid carcinoma diagnosed as a metastasis to the anterior mediastinum. Our patient has been well without the appearance of primary thyroid carcinoma in 2 years since her surgery. Whether or not occult thyroid carcinoma should be treated with thyroidectomy is controversial, and the further accumulation of experience on occult thyroid carcinoma is required.
CONFLICTS OF INTEREST STATEMENT
The authors have received no internal or external funding for this report. There are no financial disclosures. No potential conflicts of interest are declared. The patient gave her written consent for this report.



