-
PDF
- Split View
-
Views
-
Cite
Cite
Adriano Marques, Rita Camarneiro, Regina Silva, Ana Rodrigues, Isabel Dionísio, Ágata Ferreira, Margarida Brito e Melo, Laparoscopic deroofing of a ruptured hepatic cyst presenting as an acute abdomen, Journal of Surgical Case Reports, Volume 2019, Issue 2, February 2019, rjy347, https://doi.org/10.1093/jscr/rjy347
Close - Share Icon Share
Abstract
The rupture of a nonparasitic hepatic cyst is a rare complication for which there is no optimal treatment strategy yet. Laparoscopic deroofing is the standard approach for the elective treatment of symptomatic NHCs but it has seldom been described as an option for a ruptured hepatic cyst. The authors report a case of a male patient presenting to the emergency room with an acute abdomen caused by the rupture of a hepatic cyst. The patient was successfully treated by urgent laparoscopic deroofing of the cyst. Laparoscopic surgery can be a valid option for treating urgent cases presenting the same efficacy and less morbidity than open surgery.
INTRODUCTION
Nonparasitic hepatic cysts (NHCs) are a common benign liver disease, that occur in approximately 1–5% of the population and are found more frequently in women (3:1) [1]. Usually they are asymptomatic and can be managed conservatively, but about 5% of NHCs become large and symptomatic, causing abdominal pain, bloating, nausea, vomiting and dyspnoea. Those becoming symptomatic may require treatment and various procedures have been proposed such as aspiration, sclerotherapy, deroofing, enucleation or hepatectomy [2, 3].
NHCs are also associated with a variety of complications, including rupture, infection, obstructive jaundice and bleeding [1, 4].
There are very few cases of NHC rupture reported in the literature, therefore the optimal treatment strategy is yet to be defined [1, 3].
CASE REPORT
A 48-year-old male was admitted to the emergency department of our hospital complaining of a sudden onset of diffuse abdominal pain, nausea and vomiting. The patient denied recent abdominal trauma but mentioned a mild upper abdominal contusion 15 days prior to the onset of symptoms. His past medical history included a sleeve gastrectomy for morbid obesity, traumatic amputation of the left leg and asthma. Drug history on admission included asthma medication only.
On clinical examination he was distressed, his abdomen was slightly distended with diffuse tenderness, guarding and rebound tenderness. Bowell sounds were present. His blood pressure was 137/81 mmHg, pulse rate 77 beats/minute and body temperature 38.1°C. The rest of the clinical examination was unremarkable. Blood tests showed acute inflammation, with a white cell count of 12 800 × 103/μl, with 90.2% neutrophils, C-reactive protein of 5.9 mg/dl and a haemoglobin of 13.4 g/dl. Hepatobiliary and pancreatic enzymes were normal. The INR was 1.2. Chest and abdominal radiographs were normal. Computed tomography (without intravenous contrast) revealed a 9 cm hypodense lesion in segment VI of the liver and free fluid in the peritoneal cavity (Figs 1 and 2).
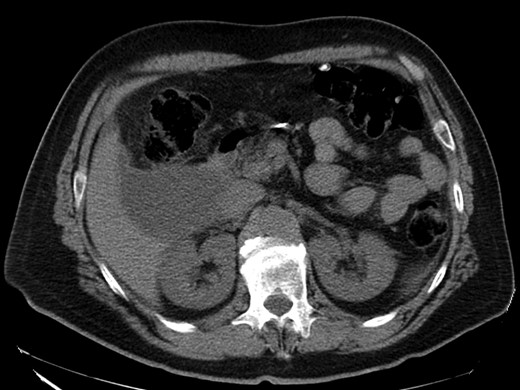
CT scan—axial view: hypodense lesion in segment VI of the liver.

CT scan—coronal view: hypodense lesion in segment VI of the liver.
Based on the patient’s clinical, laboratorial and radiological findings (acute abdomen and free peritoneal fluid of unknown origin), we proceeded with an exploratory laparoscopy.
After placing a 10 mm umbilical port, we found signs of diffuse peritonitis and a dark brown ascites throughout the abdominal cavity, but mainly in the right quadrants, from the subdiaphragmatic to the pelvic region. The source of the ascites was a large cystic lesion in segment VI of the liver that ruptured next to the gallbladder infundibulum (Fig. 3). There was no visible blood, bile or pus, and the rest of the abdominal exploration was unremarkable. After placing three additional 5 mm ports (two in the right upper quadrant and one subxiphoid), we proceeded with the deroofing of the ruptured cyst using a laparoscopic vessel-sealing device (Figs 4 and 5). The inner surface of the cyst was carefully inspected and no cystobilliary communication was found. Samples of the ascites were sent for citology and microbiology. A thorough peritoneal lavage was performed, and the abdominal cavity was drained using two 15Fr Blake drains. The total operative time was 95 min and there was a minimal blood loss.
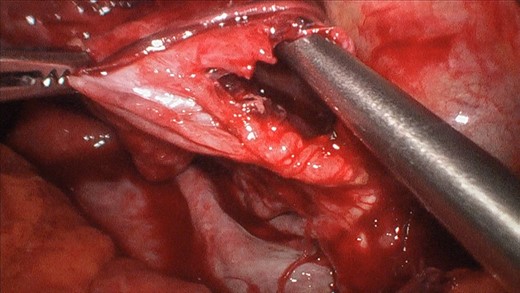
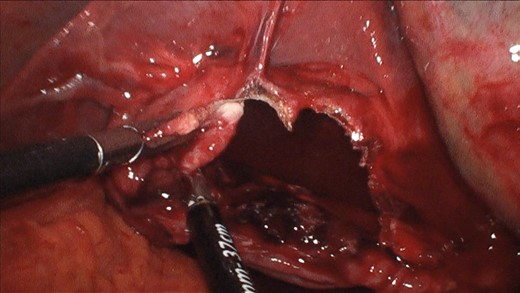
Laparoscopic deroofing of the cyst using vessel-sealing device.
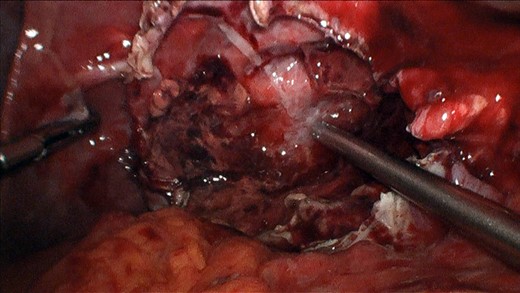
The patient was discharged 4 days after surgery without complications. The microbiology and cytology of the ascites were both negative for bacteria and cancer cells. The pathological examination of the cyst wall revealed a columnar epithelium, without dysplasia. Tumour markers were normal and Echinococcus serology was negative. Magnetic resonance imaging performed 3 months after surgery revealed a smaller 3 cm cyst at the segment VI/VII of the liver. The patient is asymptomatic.
DISCUSSION
NHC rupture is rare and its causes are variable and include infection, trauma, haemorrhage, iatrogenic injury and spontaneity [4–6].
We have described a rare case of NHC rupture, presenting as an acute abdomen. Imaoka et al. identified 19 reports describing NHC rupture and to our knowledge there are only other four cases presenting as an acute abdomen [7]. We believe that in our case, rupture was probably secondary to intracystic bleeding caused by the mild abdominal trauma that occurred two weeks prior to the onset of symptoms. We suspect that intracystic bleeding increased the tension on the cyst wall and that led to secondary rupture. The cystic fluid is usually clear and non-toxic to the peritoneum [4, 8] but in this case, it was dark brown, and it induced peritonitis. This supports the hypothesis of intracystic bleeding leading to the rupture.
Optimal treatment strategy and surgical indications for NHC rupture are not clearly defined. Some patients can be managed with a conservative approach but those unstable or presenting an acute abdomen should undergo urgent surgical intervention. This was the case with our patient, who presented with signs of diffuse peritonitis.
In the cases of NHC rupture reported there were several treatment modalities used, from conservative therapy, to drainage, sclerotherapy, transcatheter arterial embolization, cystectomy, cyst deroofing by laparoscopy or open surgery, cystectomy and hepatectomy [1]. Cyst deroofing is the treatment of choice for symptomatic non-ruptured NHCs and the laparoscopic approach is increasingly being used worldwide. The basis for using laparoscopic surgery comes from the published evidence showing lower morbidity than open approach [2]. More radical approaches have been used, with lower recurrence rates, but at the cost of higher morbidity [5, 7].
Despite having an acute abdomen, we decided for a laparoscopic approach, given that the patient was stable and that we did not know the cause for the peritonitis. Since the hepatic cyst was in segment VI, had a large extra-hepatic component and there was no evidence of active bleeding, we were able to perform the deroofing and complete the procedure by laparoscopy.
This approach might not be suitable for all cases, especially for unstable patients (bleeding or septic), cysts located in the upper and posterior segments of the liver (difficult access) and those with a biliary communication. There are only three other cases reported using laparoscopic surgery as an emergency procedure [1, 3, 9].
In conclusion, urgent laparoscopic deroofing is a valuable option for selected cases, offering the best compromise between efficacy and safety.
Conflict of Interest statement
None declared.



