-
PDF
- Split View
-
Views
-
Cite
Cite
Kyle Andrews, Andrea Rowland, Jason Tank, Knee locked in flexion: incarcerated semitendinosus tendon around a proximal tibial osteochondroma, Journal of Surgical Case Reports, Volume 2019, Issue 2, February 2019, rjy346, https://doi.org/10.1093/jscr/rjy346
Close - Share Icon Share
Abstract
This case reports on a knee locked in flexion due to incarceration of the semitendinosus tendon around an osteochondroma in a patient with a history of multiple hereditary exostoses (MHE). An 18-year-old female with history of MHE presented with acute right medial knee pain and inability to extend her knee. Radiographs confirmed multiple lower extremity osteochondromas, notably a large, 3-cm pedunculated osteochondroma about her right medial proximal tibia. This was assessed as a locked knee secondary to incarcerated hamstring tendons around an osteochondroma. Excision of the osteochondroma restored normal flexion and extension of her knee. At the 3-month follow-up visit, she had returned to all activities with no recurrent medial knee pain or locking. The differential diagnosis for a locked knee joint can be broad, but tendon incarceration should be considered in appropriate patients with significant symptoms. In patients with a history of MHE, osteochondromas may be the cause of tendon entrapment.
INTRODUCTION
‘Locked’ knee describes a knee that can flex, but is unable to fully extend [1, 2]. Attempts to passively overcome the limitation are often unsuccessful and result in pain. ‘True locking’ refers to an intra-articular mechanical block preventing knee extension, whereas ‘pseudo-locking’ is a mechanical block with an unidentified source, but often results from hamstring muscle spasm [1]. While common causes of ‘true locking’ include bucket-handle meniscal tears, cruciate ligament ruptures, or loose bodies, there are numerous case reports identifying less common causes of knee locking.
Multiple hereditary exostosis (MHE) is an autosomal dominant disorder characterized by two or more benign cartilage-capped bony tumors. In young patients, bony exostoses form within the perichondrium at the growth plates of long bones, ribs, hips and vertebrae. The perichondrium of the osteochondroma is continuous with the periosteum of the underlying bone which can be visualized with computed topography (CT) or magnetic resonance imaging (MRI) to confirm the diagnosis [3, 4]. When the physes close, these tumors cease to grow [4–7]. Due to the involvement of the physes, MHE may result in several defects, ranging from skeletal bowing, growth variance or impingement of surrounding soft tissues [7–9].
This case describes a patient with MHE who presented with her knee locked in flexion due to the incarceration of the semitendinosus tendon around an osteochondroma.
CASE DESCRIPTION
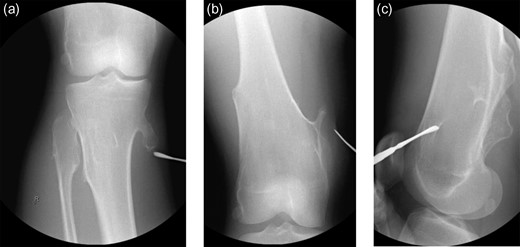
The patient is an 18-year-old female with history of MHE with many osteochondromas throughout her lower extremities who presented with acute right medial knee pain and inability to extend her knee, locked in a flexed position. The patient reports squatting in deep flexion when she felt a pop on the medial aspect of her right knee resulting in an acute inability to actively, passively or forcefully extend her knee past 90° of flexion. She has a remote history of fracture involving a right medial proximal tibial osteochondroma that has since healed uneventfully. On examination, there was tenderness localized to the medial hamstrings and soft tissues around her medial proximal tibial osteochondroma. Neurovascular function was intact. Forced knee extension could not overcome the locked knee joint and caused significant pain over the medial proximal tibia and along her hamstrings. Her patella–femoral joint was well-aligned, and she was non-tender over the anterior knee nor the medial/lateral joint lines. She had no knee effusion. Initial radiographs (Fig. 1a–c) confirmed multiple lower extremity osteochondromas, notably with a large, pedunculated osteochondroma at her right medial proximal tibia, well-healed since her previous fracture. No advanced imaging studies were performed as clinical concern for intra-articular pathology was low and patient positioning prohibited. Assessment was a locked knee secondary to incarcerated hamstring tendons around her longstanding right medial proximal tibial osteochondroma. Operative intervention was planned for excision of the osteochondroma and exploration of the soft tissues.

(a–c) Presenting radiographic images with knee locked in flexion.
The procedure began with examination under anesthesia—the right leg could be forcefully extended but resulted in significant tension about the posteromedial soft tissues of the leg. The limb was circumferentially prepped and draped in the standard orthopedic fashion without the use of a tourniquet. The osteochondromas were localized (Fig. 2a–c) and exploration revealed a bursa superficial to the osteochondroma. The gracilis tendon was in its appropriate anatomic position cranial to the pedunculated osteochondroma. The semitendinosus tendon was incarcerated inferior to the osteochondroma (Fig. 3a), creating the locked knee effect. The hooked tendon was protected, and the 3 cm osteochondroma (Fig. 3b) was removed with an oscillating saw, freeing the entrapped tendon and restoring normal movement of her knee. Radiographic imaging (Fig. 4a and b) confirmed satisfactory removal of the lesions, and the wounds were closed. At the 3-month follow-up, the patient had returned to all desired activities with no recurrent medial knee pain or locking.
(a–c) Initial intraoperative radiographic images obtained to locate the lesions.
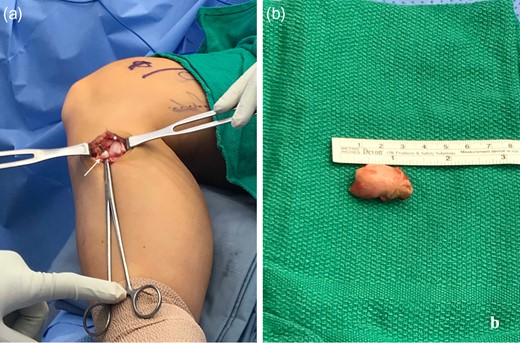
(a) Intraoperative photo demonstrating right medial proximal tibial osteochondroma (distal to *) with incarcerated semitendinosus tendon (arrow, tendon hooked by instrument) inferiorly. (b) Excised right medial proximal tibial osteochondroma.
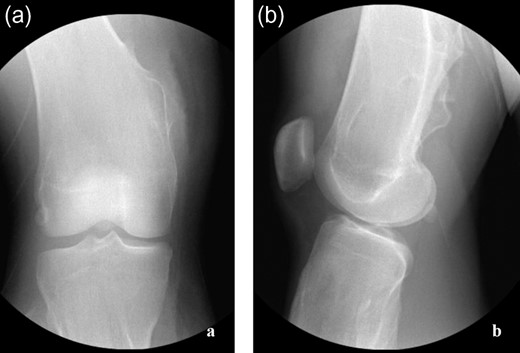
(a and b) Post-operative radiographs confirming adequate lesion excision about proximal tibia and distal femur.
DISCUSSION
A locked knee can occur suddenly, significantly interfering with daily activities due to pain and movement limitations. Bansal et al. describes a ‘triad’ for clinical recognition of a mechanical locked knee: joint line tenderness, history of definitive injury and presence of effusion. Imaging studies including radiographs, MRI or arthroscopy can confirm etiology and guide treatment [2, 10]. Intra-articular injury or tumors are typically identified as the mechanical causes of a locked knee, including meniscal pathology, cruciate injury and loose bodies [1]; less common causes include synovial hemangiomas, giant cell tumors, gouty arthropathy, fat pad cysts or intra-articular ganglion. While extra-articular causes of locked knee are less common, the patient’s history of MHE kept osteochondroma-related tendon impingement high on the differential diagnosis.
MHE is associated with benign bony projections commonly found at the metaphyses of the distal femur and proximal tibia, as seen in our patient [3, 9]. This condition is typically diagnosed in the first decade of life; lesions enlarge proportionally with overall growth rate of the individual, and cessation of growth occurs after skeletal maturity and closure of the growth plates [5]. These cartilage-capped exostoses are either sessile (broad-based) or pedunculated (stalk-like), the latter being more susceptible to traumatic injury due to weakness at the stalk [3, 5, 9].
Treatment is typically only indicated if these tumors become symptomatic. While benign, these bony protrusions can frequently cause pain and cosmetic disturbances. Mechanical effects from muscle or tendons popping or snapping as the soft tissues glide over the bony lesion have frequently been reported [5]. This repeated motion can lead to chronic irritation, entrapment, tendon ruptures or bursa formation [4, 7, 9]. Bursae can become inflamed, infected or hemorrhagic, resulting in pain. As osteochondromas do not development after skeletal maturation, any new signs of growth on imaging or new pain at sites of bony lesions should be investigated for malignant potential [4, 6, 7]. Patients with MHE have a reported rate of 5–10% of malignant degeneration into secondary chondrosarcomas [6]. Thickness of the cartilaginous cap >1.5 cm is considered suspicious for malignant transformation [4, 7, 9].
This case illustrates a unique extra-articular cause of a locked knee in flexion in a patient with MHE. After removal of the pedunculated medial proximal tibial osteochondroma, the incarcerated semitendinosus tendon was replaced to the normal anatomic position and symptoms resolved. The differential diagnosis for a locked knee joint can be quite broad, but tendon incarceration should be considered in appropriate patients with significant symptoms.
Conflict of Interest statement
None declared.



