-
PDF
- Split View
-
Views
-
Cite
Cite
Jeong-moh J Yahng, Lei Ying, When size does not matter: a rare case of popliteal artery aneurysm presenting with foot drop and its endovascular management, Journal of Surgical Case Reports, Volume 2019, Issue 12, December 2019, rjz373, https://doi.org/10.1093/jscr/rjz373
Close - Share Icon Share
Abstract
Popliteal artery aneurysms (PAA) are the commonest arterial aneurysm of the periphery. It is defined as focal dilation more than 50% of the normal vessel diameter, which usually varies between 7 and 11 mm. The most common presentation for PAA is claudication due to luminal stenosis caused by mural thrombus or acute limb ischaemia due to thromboembolism. It is much less common for patients to present with mass effect symptoms due to compression of adjacent structures, and of these, common peroneal nerve compression is particularly uncommon. We present a rare case of a 92-year-old female presenting with 4-month history of left foot drop with radiological evidence of common peroneal nerve compression secondary to PAA measuring 22 × 21 mm in size. To the best of our knowledge, this is the smallest reported popliteal aneurysm presenting with foot drop. We also present the endovascular treatment option used.
INTRODUCTION
Popliteal artery aneurysms (PAA) are the commonest arterial aneurysm of the periphery. It is defined as focal dilation of the artery more than 50% of the normal vessel diameter, which usually varies between 7 and 11 mm. PAA are associated with abdominal aortic aneurysms 40–50% of the time [1]. The commonest presentation for PAA is claudication due to luminal stenosis caused by mural thrombus or acute limb ischemia due to acute thrombosis or distal thromboembolism [2]. It is much less common for patients to present with mass effect symptoms due to compression of adjacent structures.
CASE REPORT
A 92-year-old female, independent from home, presented after multiple falls due to a four-month history of left foot drop. The foot drop had gradually worsened to the point that there was complete paralysis of ankle dorsiflexion and was associated with significant oedema of the foot. On examination, there was a large pulsatile mass in the popliteal fossa bilaterally. All peripheral pulses were palpable without any signs of ischemia. The most striking examination finding was complete paralysis of left ankle dorsiflexion with 0 out of 5 power. Ultrasound revealed that there were (Fig 1) bilateral popliteal artery aneurysms, which was larger on the left, causing displacement and impingement of the common peroneal nerve at the knee crease (Fig 2). Further computed tomography angiogram demonstrated an unruptured left PAA measuring 22 × 21 mm in maximal dimension over a distance of 24 mm (Fig 3). Intraluminal thrombus was also noted with 60% luminal stenosis. Distally, the arteries were heavily calcified with two-vessel runoff at the ankle. An emergency endovascular repair of the left PAA was performed by using 8 mm × 15 cm and 7 mm × 10 cm Gore Viabahn stents (Fig 4). The stents were deployed after a balloon-angioplasty and adequate decompression of the aneurysm was achieved. The postoperative period was uneventful, and patient’s pre-existing aspirin was continued. The leg and foot oedema improved rapidly over the subsequent few days. At follow-up in 12 weeks, the patient showed some return of motor function of the ankle and was walking with ankle splint. Her left leg remained well perfused with palpable pulses.
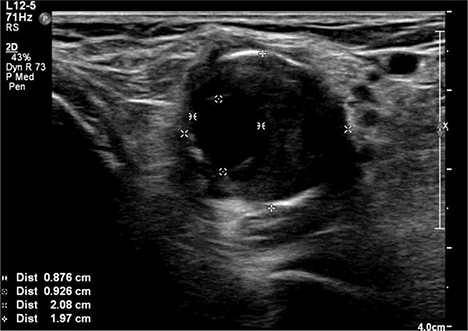
Ultrasound image of left popliteal artery aneurysm containing intramural thrombus, measuring 21 × 20 mm.
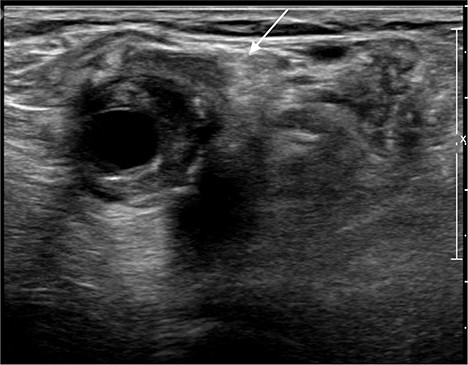
Ultrasound image of left popliteal artery aneurysm, causing displacement and impingement of the common peroneal nerve (indicated by the white arrow).
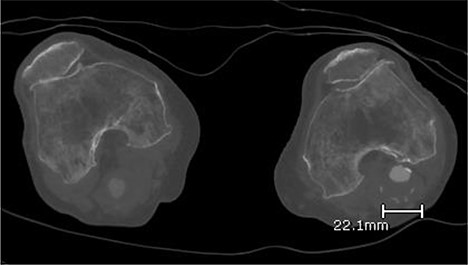
Computed topography angiogram image of left popliteal artery aneurysm, measuring 21 × 22 mm (AP × RL).

Digital subtraction angiogram image of the endovascular repair of left popliteal artery aneurysm with 8 mm × 15 cm and 7 mm × 10 cm Gore Viabahn stents.
DISCUSSION
PAA are the commonest peripheral arterial aneurysms that are often associated with abdominal aortic aneurysm [1]. PAA tend to present with symptoms of ischaemia with claudication being the most frequent presentation [2]. Non-ischaemic presentations of PAA are less common and can sometimes provide diagnostic challenges. These non-ischaemic presentations are due to compression of adjacent nerves and veins from the mass effect of PAA [2]. The structures usually involved are popliteal vein and tibial nerve due to their anatomical proximity to the popliteal artery, and they tend to present with swelling, pain and, rarely, venous thromboembolism from popliteal vein compression, or with muscle atrophy, paraesthesia and pain from tibial nerve compression [3]. Even though common peroneal neuropathy is the most common compressive mononeuropathy of the lower limb [4], it being due to PAA is rare as the two structures are relatively distant from each other. Therefore, the size of such PAA tends to be very large to cause symptoms of common peroneal nerve compression [5].
In our case, a 92-year-old, thin patient with body mass index of 19 presented with foot drop associated with leg swelling, which was initially thought to be due to deep vein thrombosis. What was interesting was that the size of the PAA was not particularly large at all; only 22 × 21 mm. To the best of our knowledge based on our extensive literature review, we believe that our case is the smallest PAA that has been reported so far to present with the symptoms of common peroneal nerve compression. Therefore, this raises an argument that the absolute size of the PAA may not always be an accurate predictor of whether a patient will have compressive symptoms from PAA. We believe that each patient’s individual anatomy should to be taken into consideration.
The general consensus across the literature regarding the indication for treatment of PAA includes asymptomatic PAA with diameter >2 cm, and all symptomatic PAA regardless of size [2, 5–7]. Until recently, it was thought that open repair was the mainstay of treatment in PAA due to the anatomical location of PAA at the knee joint, which may kink endografts during knee flexions, leading to increased risk of endograft migration, thrombosis, or even the fracture of the endograft [5]. However, with improved skill set of the endovascular interventionists and enhanced quality of new endografts, it is now becoming more evident that endovascular stents for PAA are viable treatment option for PAA in selected patients without acute limb ischaemia as they have been shown to provide excellent long-term patency and limb salvage rates [8–10].
In our case, we have opted to treat the patient’s PAA with an endovascular stent due to patient’s age and anaesthetic risks, as it allowed treatment under local anaesthetics. Our choice of the endovascular stent was based on recent advancements in endoprosthesis technology, which have led to the development of flexible self-expanding covered stents like the Viabahn and Hemobahn (W. L. Gore & Associates Inc.). These stents are pliable yet has the radial stiffness to allow their successful usage in the popliteal region [8]. Antonello et al. [10], in their 8-year prospective comparative study, demonstrated that the long-term results for asymptomatic PAA > 2 cm treated using Viabahn or Hemobahn endografts compared to open repair were comparable [10].
Many believe that PAA need be excised for successful treatment; however, we believe that it is the decompression of PAA that is the key treatment factor, especially in patients presenting with compressive symptoms. By diverting the blood flow away from the aneurismal sac, the aneurism will rapidly decompress and shrivel in size, and we speculate that is the potential explanation for the rapid improvement of leg swelling from the decompression of popliteal vein. We believe that unless there are absolute contraindications or unfavourable anatomy [10], endovascular repair of PAA is a viable and safe treatment option for PAA.



