-
PDF
- Split View
-
Views
-
Cite
Cite
Toru Nakamura, Ryo Fujikawa, Yoshifumi Arai, Yoshiro Otsuki, Kazuhito Funai, Palliative fenestration for a symptomatic subcarinal bronchogenic cyst by the prone position approach, Journal of Surgical Case Reports, Volume 2019, Issue 12, December 2019, rjz372, https://doi.org/10.1093/jscr/rjz372
Close - Share Icon Share
Abstract
A complete excision is the most reliable therapy for bronchogenic cysts (BC) but is often accompanied by technical difficulties due to severe adhesions. An 83-year-old-woman with poorly controlled diabetes noted worsening upper abdominal pain after meals and paroxysmal atrial fibrillation. Magnetic resonance imaging revealed a cystic mass in the subcarinal region, and she underwent a thoracoscopic prone position surgery. The cyst wall was found to have strictly adhered to the adjacent organs, and the lesion was not amenable to a complete excision. We performed a fenestration of the cyst wall with the aspiration of an yellowish mucus content. After opening the cavity wide enough, the remnant luminal epithelium was ablated by electrocautery. Her clinical symptoms disappeared immediately after the surgery without any surgical morbidity. A prone-position thoracoscopic palliative fenestration is a feasible option for a symptomatic subcarinal BC.
INTRODUCTION
Bronchogenic cysts (BCs) arise from abnormal budding of the tracheobronchial tree and often develop in the mediastinum. A complete excision is the most reliable therapy but is often accompanied by technical difficulties due to severe adhesions especially in symptomatic patients [1]. We herein report a subcarinal BC case who successfully underwent a palliative fenestration to improve clinical symptoms by the prone-position thoracoscopic approach.
CASE REPORT
An 83-year-old-woman presented with a subcarinal mass detected by a precise examination of upper abdominal pain worsening after meals. Magnetic resonance imaging revealed a well-circumscribed cystic mass in the subcarinal area compressing the surrounding organs and suggested a BC as the most likely diagnosis (Fig 1). She had poorly controlled type 2 diabetes mellitus (A1c level 9.1%), hypertension, and also noted worsening paroxysmal atrial fibrillation (CHADS2 score3) and was receiving dabigatran etexilate over the last several months. A surgical resection of the cyst was recommended. With the patient in the prone position, two 5-mm ports in the third and fifth inter costal spaces (ICSs) and a 12-mm port in in the seventh ICS on the mid-axillary line were made, respectively. An additional 5-mm port was inserted into the eighth ICS on the scapular line and used as a camera port (Fig 2). Carbon dioxide (CO2) was insufflated at a pressure of 8–mm Hg and then a tense mass was clearly visualized in the subcarinal area (Fig 3). The cyst wall was found to have strictly adhered to the adjacent organs suggestive of past inflammatory events. Because an attempt to dissect between the cyst and lung resulted in parenchymal injury with alveolar leakage, we considered that the lesion was not amenable to a complete excision. After
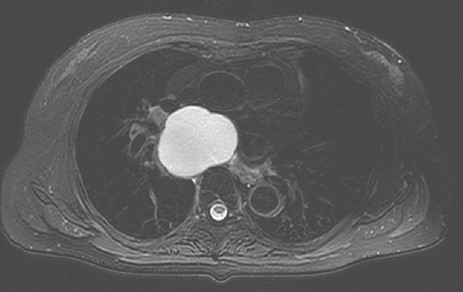
T2 weighted image showing a subcarinal cyst compressing the surrounding organs.
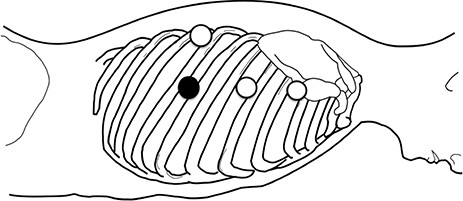
The patient position and port insertion sites; three 5-mm ports (open circles) and one 12-mm port (filled circle) were placed.
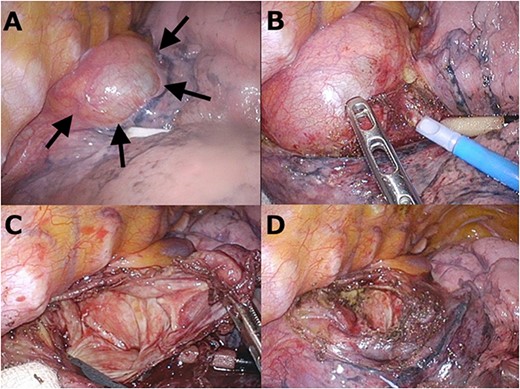
Operative view in the prone position. A: The cyst wall strictly adhered to the surrounding organs (arrows). B: An attempt of a complete resection resulted in lung injury due to the severe adhesions. C: Opening the cyst wall to adequately drain the cavity space. D: After removing a large proportion of the wall, the remnant luminal epithelium was ablated by electrocautery.
the fenestration of the cyst wall with the aspiration of an yellowish mucus content, a large proportion of the thickened wall was removed to open the cavity wide enough. The remnant luminal epithelium was ablated by electrocautery. The operative time was 117 minutes and the bleeding amount was 5 g. The postoperative course was uneventful, and she was discharged on the second postoperative day. A histopathological examination revealed a ciliated epithelium, hyaline cartilage and bronchial mucus glands consistent with a BC. Her digestive problem and palpitations disappeared immediately after the surgery, and she is currently symptom free at 18 months.
DISCUSSION
The subcarinal area is one of the most frequent sites of mediastinal BCs, and the lateral decubitus approach has been the standard surgical procedure [1, 2]. Furthermore, the prone position approach for the posterior mediastinum has broadened in use due to the recent advances in esophageal cancer surgery [3, 4]. The gravity effect combined with CO2 insufflation pulls the lungs and heart downward to facilitate a better surgical field requiring less additional retraction than the lateral approach [5]. This gravity effect with positive pressure may obviate the need for one lung ventilation and is helpful to avoid postoperative atelectasis [6]. In addition, the prone positioning also provides a better arterial oxygenation and systemic blood flow by increasing the functional residual volume [7], which might be beneficial especially in high-risk patients.
Although most BCs are asymptomatic, some patients develop a cough, pain, dyspnea or fever and it may result in severe adhesions to the surrounding organs [1, 8, 9]. While a total removal of the cyst is the mainstay of the curative therapy, a partial resection has been an alternative option in adhesive cases [10]. Our case was found to have severe adhesions, which led us to a palliative fenestration with a satisfactory outcome.
A prone-position thoracoscopic palliative fenestration is a feasible option for a symptomatic subcarinal BC with less morbidity and a satisfactory clinical outcome especially in high-risk patients.
ACKNOWLEDGEMENTS
We thank Mr. John Martin for his proof reading of the manuscript.



