-
PDF
- Split View
-
Views
-
Cite
Cite
Yukihito Kuroda, Katsuji Hisakura, Yoshimasa Akashi, Tsuyoshi Enomoto, Tatsuya Oda, A case of sigmoid colon perforation presenting with pneumomediastinum, Journal of Surgical Case Reports, Volume 2019, Issue 12, December 2019, rjz359, https://doi.org/10.1093/jscr/rjz359
Close - Share Icon Share
Abstract
A 62-year-old woman had developed polymyositis 12 years previously and had taken oral steroids. Chest and abdominal computed tomography showed pneumomediastinum and free air in the abdominal cavity. Although a colon perforation was suspected, the perforation site could not be identified on the image. In addition, a diagnosis of oesophageal rupture could not be excluded from the findings of pneumomediastinum. After general anaesthesia, an upper gastrointestinal endoscopy was performed before surgery. Because there was no obvious perforation in the oesophagus, a laparotomy approach was used. A perforation was found on the mesentery side of the sigmoid colon, and a perforation of the sigmoid colon’s diverticulum towards the mesentery was diagnosed. A Hartmann’s procedure was performed. Colon perforations are rarely associated with pneumomediastinum. Preoperative endoscopy is useful to help diagnose and determine the surgical procedure if an obvious perforation cannot be identified.
INTRODUCTION
Colon perforations rarely occur on the mesentery side, but they can progress from retroperitoneal emphysema to mediastinal and subcutaneous emphysema.
We report here the difficulty of diagnosing sigmoid colon perforation with pneumomediastinum, but preoperative upper gastrointestinal endoscopy helped us determine the surgical procedure.
CASE REPORT
A 62-year-old woman presented with a chief complaint of abdominal, back and neck pain. She had developed polymyositis 12 years previously and started taking prednisolone (controlled at 11 mg/day at the visit). She was also taking oral medication for hypertension.
Lower abdominal pain appeared a day after upper gastrointestinal angiography with barium contrast agent. Subsequently, she experienced gradual abdominal, back and neck pain. Chest and abdominal computed tomography (CT) showed mediastinal emphysema and free air in the abdominal cavity. She was referred to our hospital for suspicion of an oesophageal rupture.
The patient’s height was 152 cm, body weight was 41 kg, body temperature was 39.4 °C, blood pressure was 160/99 mmHg, and pulse rate was 140 times/minute. Her abdomen was markedly bloated with an overall rebound tenderness.
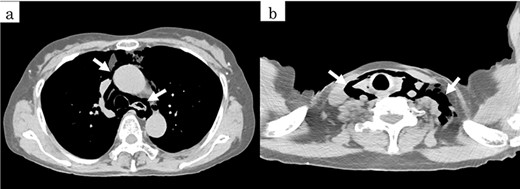
On chest and abdominal CT, free gas was observed in the entire abdominal cavity (Fig. 1a), and extensive emphysema was also observed in the retroperitoneum (Fig. 1b). In addition, it was observed from the mediastinum to both sides of the necks (Fig. 2).
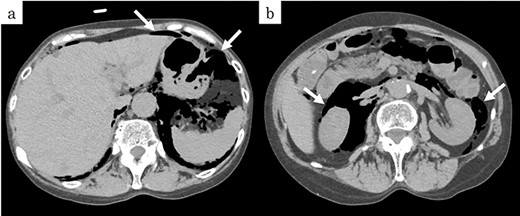
Preoperative CT showed (a) pneumoperitoneum (arrows) and (b) a massive pneumoretroperitoneum (arrows).
Colon perforation was suspected from the abdominal findings and the finding of free gas in the abdominal cavity. Although emergency surgery was planned, the perforation site could not be identified on the image. In addition, a diagnosis of oesophageal rupture could not be ruled out because of atypical findings of colon perforation, such as pneumomediastinum. Therefore, after general anaesthesia, upper gastrointestinal endoscopy was performed for the purpose of diagnosis and operative decision. Because there was no obvious perforation in the oesophagus, oesophageal rupture was ruled out, and a laparotomy approach was used.
When the abdominal midline incision was performed, extensive emphysema was observed throughout the mesentery (Fig. 3a). There was no stool-like ascites in the abdominal cavity, and a small amount of cloudy ascites was observed in the pelvis. When the serosa of the sigmoid colon, where emphysema was most prominent, was incised and observed, a perforated part was found on the mesentery side of the sigmoid colon, from which stool leakage was confirmed (Fig. 3b). The diagnosis of perforation of the sigmoid diverticulum into the mesentery was made, and a Hartmann’s procedure was performed. The histopathological diagnosis was consistent with diverticulum perforation (Fig. 4).
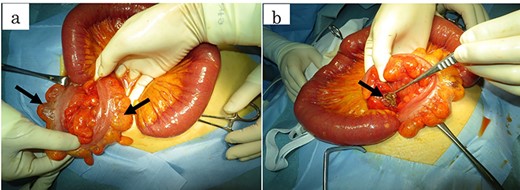
Intraoperative findings revealed (a) pneumatosis changes in the mesenterium (arrows) and (b) perforation of the sigmoid colon at the side of the intramesenteric space (arrows).
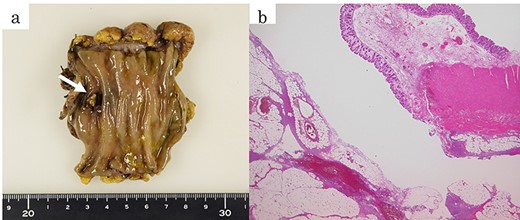
(a) The fixed sample showed a perforation site on the mesenteric side of the sigmoid colon (arrows). (b) The pathological specimen (haematoxylin and eosin, ×12.5) showed a rupture of the muscular layer, compatible with diverticular perforation.
Postoperatively, the patient was withdrawn from the ventilator on hospital Day 1. Chest and abdominal CT performed on hospital Day 8 confirmed a marked reduction in emphysema from the retroperitoneum to the mediastinum and neck (Fig. 5). The patient’s postoperative course was good, and she was discharged on hospital Day 21.
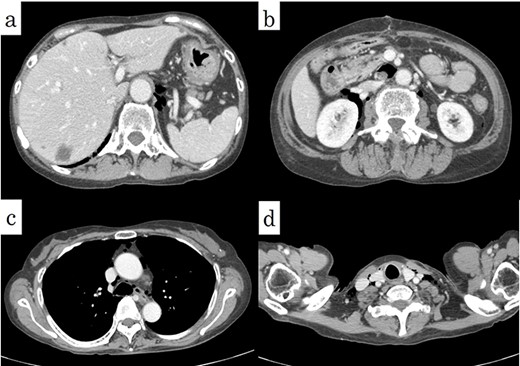
Postoperative CT showed a decrease of the pneumoretroperitoneum and pneumomediastinum (arrows).
DISCUSSION
Colonic perforation takes the form of a free perforation that occurs on the contralateral side of the mesentery and is often accompanied by severe faecal peritonitis [1]. Unlike the small intestine, which is fed from the marginal artery to the opposite side, the colon is fed by terminal arteries in which the straight arteries rarely anastomose. Therefore, the contralateral side of the mesentery is the most ischaemic region, and the colonic perforation usually takes the form of a free perforation [2]. Perforation into the mesentery is rare among colonic perforations [3]. When perforating into the mesentery, the contents of the intestinal tract are covered with the mesenchyme and are less likely to cause peritoneal inflammation, and this type of perforation is characterized by poor findings such as free gas and ascites retention [4]. Furthermore, there are cases in which perforation on the mesentery side progresses from retroperitoneal emphysema to mediastinal and subcutaneous emphysema, as in this case [5]. The mechanism is considered to be gastrointestinal gas produced from the colonic perforation into the mesentery developing towards the mediastinum via the retroperitoneum to form pneumomediastinum [6].
By searching the Japan Medical Abstracts Society from 1983 to 2018 with the keywords large intestine, rectum, and pneumomediastinum, we found 19 Japanese cases of pneumomediastinum due to perforation of the large intestine and rectum (Table 1). In three cases, the patients were undergoing steroid treatment for collagen disease. The causes of gastrointestinal perforation in patients undergoing steroid therapy for polymyositis include (1) necrosis due to submucosal tissue ischaemia caused by vascular lesions such as vasculitis and (2) steroid-induced intestinal wall weakness, ulceration, and delayed wound healing [7]. In our case, it was suggested that the perforation into the mesentery, which is rare, was related to steroid treatment.
| . | Year . | Author . | Age . | Sex . | Cause . | Site . | Underlying disease . | PSL/day . | Suffering term . | Operation . | Outcome . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2002 | Koshiko | 57 | F | Diverticulum | S | (−) | (−) | Sigmoidectomy | Alive | |
| 2 | 2003 | Ota | 80 | F | Colonoscopy | S | (−) | (−) | Hartmann | Alive | |
| 3 | 2005 | Kanehiro | 87 | M | Stercoroma | S | (−) | (−) | Hartmann | Dead | |
| 4 | 2005 | Hashimoto | 78 | F | Stercoroma | S | (−) | (−) | Colostomy | Dead | |
| 5 | 2006 | Chatani | 47 | F | Stercoroma | R | RA | 10 mg | 6 y | Hartmann | Alive |
| 6 | 2006 | Ball | 77 | F | Colonoscopy | AS | (−) | (−) | Primary closure | Alive | |
| 7 | 2007 | Matsuura | 93 | F | Colonoscopy | T | (−) | (−) | Primary closure | Alive | |
| 8 | 2009 | Aoki | 78 | M | Colonoscopy | S | RA | Unknown | Unknown | Primary closure | Alive |
| 9 | 2010 | Maruyama | 80 | M | Colon volvulus | S | (−) | (−) | Hartmann | Alive | |
| 10 | 2012 | Takashima | 67 | M | Colon volvulus | S | (−) | (−) | Hartmann | Alive | |
| 11 | 2013 | Hasuda | 72 | M | Colonoscopy | R | (−) | (−) | Hartmann | Alive | |
| 12 | 2013 | Kiyama | 28 | F | Enema | R | (−) | (−) | Colostomy | Alive | |
| 13 | 2014 | Shimoda | 78 | F | Diverticulum | R | (−) | (−) | Hartmann | Alive | |
| 14 | 2014 | Nakaji | 69 | M | Colonoscopy | A | (−) | (−) | Conservative therapy | Alive | |
| 15 | 2014 | Shinozaki | 20 | F | Trauma | R | (−) | (−) | Colostomy | Alive | |
| 16 | 2015 | Mori | 79 | M | Postoperative complication | T | (−) | (−) | Ileostomy | Alive | |
| 17 | 2016 | Fukuoka | 71 | F | Colonoscopy | S | (−) | (−) | Conservative therapy | Alive | |
| 18 | 2016 | Kawamura | 88 | M | Colon cancer | S | (−) | (−) | Hartmann | Alive | |
| 19 | 2017 | Ichikawa | 42 | M | Diverticulum | D | (−) | (−) | Left colectomy | Alive | |
| 20 | Our case | 65 | F | Diverticulum | S | PM | 11 mg | 12 y | Hartmann | Alive |
| . | Year . | Author . | Age . | Sex . | Cause . | Site . | Underlying disease . | PSL/day . | Suffering term . | Operation . | Outcome . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2002 | Koshiko | 57 | F | Diverticulum | S | (−) | (−) | Sigmoidectomy | Alive | |
| 2 | 2003 | Ota | 80 | F | Colonoscopy | S | (−) | (−) | Hartmann | Alive | |
| 3 | 2005 | Kanehiro | 87 | M | Stercoroma | S | (−) | (−) | Hartmann | Dead | |
| 4 | 2005 | Hashimoto | 78 | F | Stercoroma | S | (−) | (−) | Colostomy | Dead | |
| 5 | 2006 | Chatani | 47 | F | Stercoroma | R | RA | 10 mg | 6 y | Hartmann | Alive |
| 6 | 2006 | Ball | 77 | F | Colonoscopy | AS | (−) | (−) | Primary closure | Alive | |
| 7 | 2007 | Matsuura | 93 | F | Colonoscopy | T | (−) | (−) | Primary closure | Alive | |
| 8 | 2009 | Aoki | 78 | M | Colonoscopy | S | RA | Unknown | Unknown | Primary closure | Alive |
| 9 | 2010 | Maruyama | 80 | M | Colon volvulus | S | (−) | (−) | Hartmann | Alive | |
| 10 | 2012 | Takashima | 67 | M | Colon volvulus | S | (−) | (−) | Hartmann | Alive | |
| 11 | 2013 | Hasuda | 72 | M | Colonoscopy | R | (−) | (−) | Hartmann | Alive | |
| 12 | 2013 | Kiyama | 28 | F | Enema | R | (−) | (−) | Colostomy | Alive | |
| 13 | 2014 | Shimoda | 78 | F | Diverticulum | R | (−) | (−) | Hartmann | Alive | |
| 14 | 2014 | Nakaji | 69 | M | Colonoscopy | A | (−) | (−) | Conservative therapy | Alive | |
| 15 | 2014 | Shinozaki | 20 | F | Trauma | R | (−) | (−) | Colostomy | Alive | |
| 16 | 2015 | Mori | 79 | M | Postoperative complication | T | (−) | (−) | Ileostomy | Alive | |
| 17 | 2016 | Fukuoka | 71 | F | Colonoscopy | S | (−) | (−) | Conservative therapy | Alive | |
| 18 | 2016 | Kawamura | 88 | M | Colon cancer | S | (−) | (−) | Hartmann | Alive | |
| 19 | 2017 | Ichikawa | 42 | M | Diverticulum | D | (−) | (−) | Left colectomy | Alive | |
| 20 | Our case | 65 | F | Diverticulum | S | PM | 11 mg | 12 y | Hartmann | Alive |
S, sigmoid colon; R, rectum; AS: anastomotic site; T: transverse colon; A: ascending colon; D: descending colon; RA: rheumatism; PM: polymyositis; PSL: prednisolone.
| . | Year . | Author . | Age . | Sex . | Cause . | Site . | Underlying disease . | PSL/day . | Suffering term . | Operation . | Outcome . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2002 | Koshiko | 57 | F | Diverticulum | S | (−) | (−) | Sigmoidectomy | Alive | |
| 2 | 2003 | Ota | 80 | F | Colonoscopy | S | (−) | (−) | Hartmann | Alive | |
| 3 | 2005 | Kanehiro | 87 | M | Stercoroma | S | (−) | (−) | Hartmann | Dead | |
| 4 | 2005 | Hashimoto | 78 | F | Stercoroma | S | (−) | (−) | Colostomy | Dead | |
| 5 | 2006 | Chatani | 47 | F | Stercoroma | R | RA | 10 mg | 6 y | Hartmann | Alive |
| 6 | 2006 | Ball | 77 | F | Colonoscopy | AS | (−) | (−) | Primary closure | Alive | |
| 7 | 2007 | Matsuura | 93 | F | Colonoscopy | T | (−) | (−) | Primary closure | Alive | |
| 8 | 2009 | Aoki | 78 | M | Colonoscopy | S | RA | Unknown | Unknown | Primary closure | Alive |
| 9 | 2010 | Maruyama | 80 | M | Colon volvulus | S | (−) | (−) | Hartmann | Alive | |
| 10 | 2012 | Takashima | 67 | M | Colon volvulus | S | (−) | (−) | Hartmann | Alive | |
| 11 | 2013 | Hasuda | 72 | M | Colonoscopy | R | (−) | (−) | Hartmann | Alive | |
| 12 | 2013 | Kiyama | 28 | F | Enema | R | (−) | (−) | Colostomy | Alive | |
| 13 | 2014 | Shimoda | 78 | F | Diverticulum | R | (−) | (−) | Hartmann | Alive | |
| 14 | 2014 | Nakaji | 69 | M | Colonoscopy | A | (−) | (−) | Conservative therapy | Alive | |
| 15 | 2014 | Shinozaki | 20 | F | Trauma | R | (−) | (−) | Colostomy | Alive | |
| 16 | 2015 | Mori | 79 | M | Postoperative complication | T | (−) | (−) | Ileostomy | Alive | |
| 17 | 2016 | Fukuoka | 71 | F | Colonoscopy | S | (−) | (−) | Conservative therapy | Alive | |
| 18 | 2016 | Kawamura | 88 | M | Colon cancer | S | (−) | (−) | Hartmann | Alive | |
| 19 | 2017 | Ichikawa | 42 | M | Diverticulum | D | (−) | (−) | Left colectomy | Alive | |
| 20 | Our case | 65 | F | Diverticulum | S | PM | 11 mg | 12 y | Hartmann | Alive |
| . | Year . | Author . | Age . | Sex . | Cause . | Site . | Underlying disease . | PSL/day . | Suffering term . | Operation . | Outcome . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2002 | Koshiko | 57 | F | Diverticulum | S | (−) | (−) | Sigmoidectomy | Alive | |
| 2 | 2003 | Ota | 80 | F | Colonoscopy | S | (−) | (−) | Hartmann | Alive | |
| 3 | 2005 | Kanehiro | 87 | M | Stercoroma | S | (−) | (−) | Hartmann | Dead | |
| 4 | 2005 | Hashimoto | 78 | F | Stercoroma | S | (−) | (−) | Colostomy | Dead | |
| 5 | 2006 | Chatani | 47 | F | Stercoroma | R | RA | 10 mg | 6 y | Hartmann | Alive |
| 6 | 2006 | Ball | 77 | F | Colonoscopy | AS | (−) | (−) | Primary closure | Alive | |
| 7 | 2007 | Matsuura | 93 | F | Colonoscopy | T | (−) | (−) | Primary closure | Alive | |
| 8 | 2009 | Aoki | 78 | M | Colonoscopy | S | RA | Unknown | Unknown | Primary closure | Alive |
| 9 | 2010 | Maruyama | 80 | M | Colon volvulus | S | (−) | (−) | Hartmann | Alive | |
| 10 | 2012 | Takashima | 67 | M | Colon volvulus | S | (−) | (−) | Hartmann | Alive | |
| 11 | 2013 | Hasuda | 72 | M | Colonoscopy | R | (−) | (−) | Hartmann | Alive | |
| 12 | 2013 | Kiyama | 28 | F | Enema | R | (−) | (−) | Colostomy | Alive | |
| 13 | 2014 | Shimoda | 78 | F | Diverticulum | R | (−) | (−) | Hartmann | Alive | |
| 14 | 2014 | Nakaji | 69 | M | Colonoscopy | A | (−) | (−) | Conservative therapy | Alive | |
| 15 | 2014 | Shinozaki | 20 | F | Trauma | R | (−) | (−) | Colostomy | Alive | |
| 16 | 2015 | Mori | 79 | M | Postoperative complication | T | (−) | (−) | Ileostomy | Alive | |
| 17 | 2016 | Fukuoka | 71 | F | Colonoscopy | S | (−) | (−) | Conservative therapy | Alive | |
| 18 | 2016 | Kawamura | 88 | M | Colon cancer | S | (−) | (−) | Hartmann | Alive | |
| 19 | 2017 | Ichikawa | 42 | M | Diverticulum | D | (−) | (−) | Left colectomy | Alive | |
| 20 | Our case | 65 | F | Diverticulum | S | PM | 11 mg | 12 y | Hartmann | Alive |
S, sigmoid colon; R, rectum; AS: anastomotic site; T: transverse colon; A: ascending colon; D: descending colon; RA: rheumatism; PM: polymyositis; PSL: prednisolone.
The patient was referred to our hospital for suspicion of oesophageal rupture because of a mediastinal emphysema on CT. We could not rule out oesophageal rupture because the image was not typical of perforation of the large intestine. Therefore, we performed upper gastrointestinal endoscopy after general anaesthesia. Endoscopy has been reported to be useful for preoperative diagnosis of oesophageal rupture [8], and we usually perform endoscopy after general anaesthesia as an emergency surgery for oesophageal rupture. This procedure is intended to determine the surgical procedure and approach by identifying the perforation site before surgery, and in this case, it was also useful to diagnose and determine the surgical procedure. Although none of the previously reported cases of pneumomediastinum due to perforation of the large intestine and rectum were suspected to involve oesophageal rupture prior to surgery, preoperative endoscopy should be performed because there are some reports of oesophageal rupture with free gas in the abdominal cavity [9].
In previous reports, pneumomediastinum due to perforation of the large intestine and the rectum was not associated with mediastinitis. It is reported that pneumomediastinum associated with perforation of the large intestine can improve without surgical drainage of the mediastinum [10]. By performing preoperative endoscopy, we confirmed that there was no perforation of the oesophagus and surgery was performed using only the lower abdominal laparotomy approach without any significant invasion such as thoracotomy.
Conflict of Interest statement
None declared.



