-
PDF
- Split View
-
Views
-
Cite
Cite
Manuel Jaklitsch, Mafalda Sobral, António Augusto Ferreira Pinto de Figueiredo, Americo Martins, Hugo Pinto Marques, Rare giant: mature cystic teratoma in the liver, Journal of Surgical Case Reports, Volume 2019, Issue 12, December 2019, rjz347, https://doi.org/10.1093/jscr/rjz347
Close - Share Icon Share
Abstract
Teratomas are rare pluripotent embryonic tumours occurring mostly in gonadal organs and pediatric age groups. Mature cystic teratoma in the liver are rare, and to the best of our knowledge, only a dozen cases in adults have been published in the literature. We present a 27-year-old female who had a history of loss of appetite and mild abdominal distention. Computed Tomography revealed a liver mass suggestive of teratoma. The patient underwent elective surgery, and the diagnosis of mature cystic liver teratoma was confirmed histologically. Measuring 23 cm in a longitudinal axis, the patient had an uneventful post-operative evolution and was discharged on day eight. Teratomas in the liver are a rare finding, especially in adults, mostly due to their asymptomatic evolution. Due to the possibility of malignant transformation, complete surgical resection remains the best treatment option.
INTRODUCTION
Teratomas are rare pluripotent embryonic tumours, occurring mostly in gonadal organs [1]. The term derives from the Greek ‘teratos’ meaning monster [2]. By definition, it must contain at least two of three germ layers: ectoderm, mesoderm and endoderm [2, 3]. To the best of our knowledge, <50 cases of primary hepatic teratomas have been reported, the majority in the pediatric age group, and only a dozen case reported for adults [4]. Encountered predominantly in the female population, [1, 5] teratomas possess distinctive imaging characteristics which allow accurate pre-operative diagnosis in most cases. Histological examination permits a definitive diagnosis along with the assessment of maturity [6].
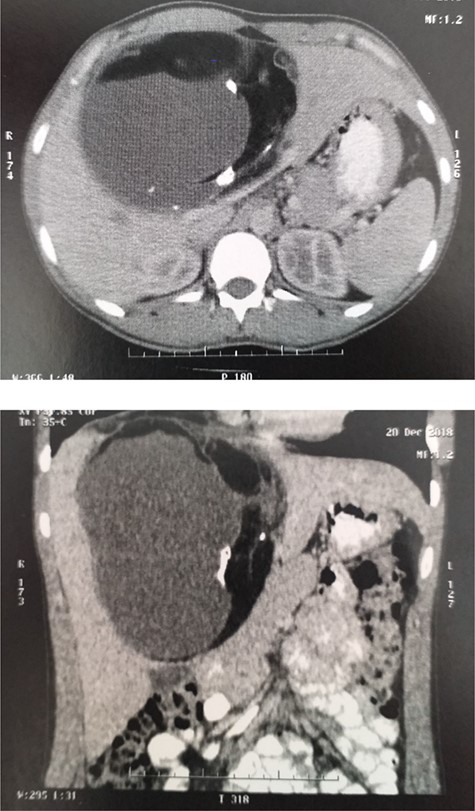
Enhanced CT: ill-defined contrast-enhancing, multilobulated cystic lesion involving segments II, III, VI and VIII.
CASE REPORT
This is a case of a 27-year-old female who presented with 3 months of loss of appetite associated with mild abdominal distension and a sense of fullness in the right upper quadrant. She had no significant past medical history, with a cigarette smoking habit of consuming one pack per year. On physical examination, no icterus was noted. Mild distention in the right superior quadrant of the abdomen was recognized, a tender and smooth-surfaced mass was identified by liver palpation. Routine clinical investigation revealed a carcinoembryonic antigen of 6.5. All other haematological and biochemical parameters were within the reference range. An abdominal contrast-enhanced computed tomography (CT) showed an ill-defined contrast-enhancing, multilobulated cystic lesion involving segments II, III, VI, VIII measuring 19 × 15 × 10 cm, containing adipose tissue with calcifications and multiple septations (Fig. 1). These findings were suggestive of teratoma. Beta human chorionic gonadotropin and Echinococcus serology were negative. Intraoperatively, a well-defined cyst was confirmed occupying segments IV, V, VIII and partially segments II and III; a mesohepatectomy and cholecystectomy were performed (Fig. 2) with two 15-minute pedicular clampages (Pringle manoeuvre). The right and left hepatic veins were exposed. Due to compression and distortion of the structures, inadvertent opening of the anterior sectorial biliary branch occurred. As a small amount of parenchyma was still draining through this duct, a reconstruction via a Roux-en-Y Hepatico-Yeyunostomy was performed. The patient had an uneventful postoperative evolution, dispatched on day eight. Histopathology reported a surgical specimen with a weight of 1837 g with the dimensions 21 × 18 × 12 cm. The outer surface was smooth and yellowish-grey in colour. The cystic wall had a pattern of irregular thickness, with a maximum thickness of 2 cm with calcified multilobulated areas, containing yellowish sebum paste and hair, the diagnosis was mature cystic teratoma (MCT) (Fig. 3). In subsequent follow-up, patient reintegrated actively in her socio-laboral environment.
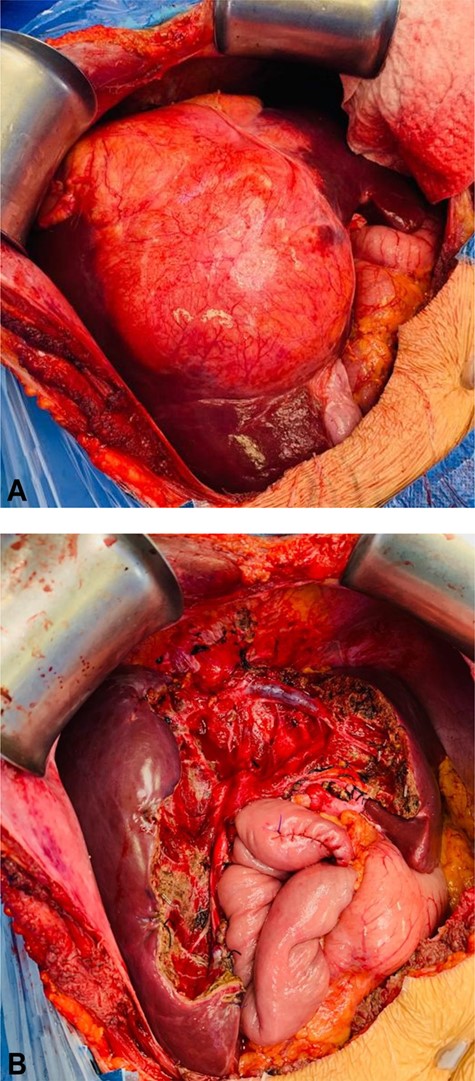
(A) In situ mass, occupying segments II, III, VI, V and VIII. (B) Post resection, visualizing right and left suprahepatic vein, and Y-Roux hepaticojejunostomy.
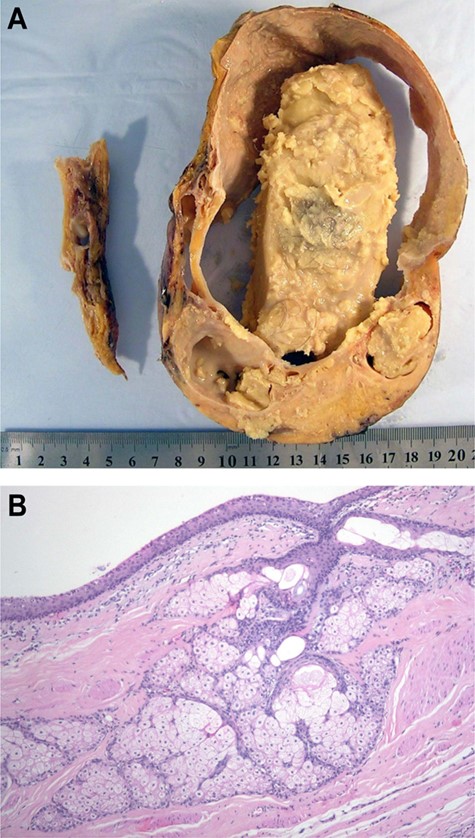
(A) Macroscopic specimen. (B) Microscopic slice where hair and skin tissue are appreciated.
DISCUSSION
Hepatic teratoma is a rare finding; to the best of our knowledge, only a small number of case reports are present in the literature, and no liver-specific treatment guidelines have been established [2, 4, 5]. The largest tumour recorded to date measured 27 cm in diameter [7]. Teratomas usually occur, in declining order of frequency, in the ovaries, testes, anterior mediastinum, retroperitoneum, sacrococcygeal region and cranium [1, 2]. The involvement of mesentery and gastrointestinal tract are rare, and they are most commonly found in children, with only a few cases reported in adults [8]. Teratomas of the liver account for <1% of all teratomas. It is believed that during the period of organogenesis, the arrest in migration along the urogenital ridge can lead to the development of teratomas in extra-gonadal sites; [1, 5] the hypothesis of re-implantation of ovarian teratoma in an extra-gonadal site has also been proposed. [4] MCT are known to have a slow growth rate (<2 mm/y) [8]. The characteristic imaging appearance of an MCT in CT is a cystic mass containing adipose sebaceous fluid, mostly unilocular with a distinct surrounding capsule, a differential diagnosis with other fat-containing liver masses including myelolipoma, lipoma, angiomyolipoma, and metastatic adipose tumour of the liver should be made [9]. Magnetic resonance imaging has also been proven to be a viable imaging modality, [2] while fluorodeoxyglucose (FDG) positron emission tomography has limited diagnostic use to the low FDG uptake presented by MCT [10]. The definitive diagnosis of MCT is possible through histological examination, characteristically containing variable amounts of calcification (56%) such as bone, teeth, hair or soft and fat (93%) neural tissue and rarely thyroid and pancreatic tissue [4, 8]. The presence of immature tissue in any of their germ layers influences an unfavourable prognosis, which is based on the histopathological features categorized in benign and malignant [5]. The rate of malignant transformation of teratomas has been reported ranging from 2% to 3%, more commonly encountered in children, and although malignant transformation within cystic teratomas most commonly involves squamous cell carcinoma (80%), others such as adenocarcinoma (6.8%), sarcomas and carcinoid tumours may occur as well [1]. Concerning findings include the invasion of adjacent structures and irregular wall thickening. For unknown reasons, they are more common in females and the right hepatic lobe [2]. Usually, hepatic teratomas are well-defined encapsulated lesions, with diminishing complexity in resection from surrounding hepatic parenchyma [5].
CONCLUSION
MCT is a rare condition in adults that needs to be considered in the differential diagnosis of solid-cystic neoplasms in the liver. Surgical resection remains the mainstay of management and risk stratification based on histology should determine postoperative surveillance.
CONFLICTS OF INTEREST
The author has no conflicts of interest to declare.



