-
PDF
- Split View
-
Views
-
Cite
Cite
Majid Z Albeeshi, Abdullah A Alwanyan, Alaa A Salim, Ibrahim T Albabtain, Appendiceal diverticulitis presenting as acute appendicitis diagnosed postoperatively, Journal of Surgical Case Reports, Volume 2019, Issue 12, December 2019, rjz332, https://doi.org/10.1093/jscr/rjz332
Close - Share Icon Share
Abstract
Appendiceal diverticular disease is a rare entity. We report a case of appendiceal diverticulitis mimicking acute appendicitis and diagnosed postoperatively on histopathology. A 28-year-old female presented with a 2-day history of shifting periumbilical pain associated with nausea and anorexia. A computed tomography scan of the abdomen demonstrated acute appendicitis. She was taken to laparoscopic appendectomy. Histopathology showed appendiceal diverticulitis, and perforation of an inflamed diverticulum with periappendicitis. Diverticulosis of the appendix is classified as congenital and acquired. Diagnosis can be made preoperatively by imaging. In this case, diverticulosis was not radiologically evident, and was interpreted as acute appendicitis. Gross appearance of the resected appendix was not suggestive of diverticulitis. Other cases reported that the gross specimen had evidence of diverticular disease. Surgeons should be aware that inflamed appendixes may harbor different pathologies warranting further management.
INTRODUCTION
Appendiceal diverticular disease is a rare entity. The first description of appendiceal diverticulosis was published by the pathologist Kelynack in 1893 [1]. The reported prevalence is between 0.014 and 3.7% in some studies [2–4]. It is diagnosed preoperatively, often based on clinical picture only, with diagnosis usually confirmed at pathology. Acute appendicitis is the most common pathology of the appendix. Both acute appendicitis and appendiceal diverticulitis can present with right lower quadrant pain, which makes them difficult to differentiate clinically.
This condition can be associated with neuroendocrine tumors (carcinoids), mucinous adenomas, tubular adenomas and adenocarcinomas [5]. There is no association between colonic diverticulosis and appendiceal diverticulosis [2]. We report a case of appendiceal diverticulitis mimicking acute appendicitis and diagnosed postoperatively based on histopathological features.
CASE PRESENTATION
A 28-year-old female presented to the emergency department with a 2-day history of periumbilical pain, shifting to the right lower quadrant, associated with nausea and anorexia. She also reported burning micturition with no other changes in urine. There was no fever, weight loss or change in bowel habits.
Her medical history was significant for polycystic ovary syndrome, on cyproterone acetate and ethinyl estradiol (Diane-35), and subclinical hypothyroidism. She had no previous surgical history. Last menstrual period was 3 weeks prior to presentation. On physical examination, she was afebrile and hemodynamically stable. Her abdomen was soft and not distended. There was tenderness at the right lower quadrant with positive rebound tenderness. There was no guarding or rigidity. Rovsing, obturator and psoas signs were negative.
A pelvic ultrasound was normal. Gynecological causes of pain were ruled out. A computed tomography (CT) scan of the abdomen and pelvis demonstrated acute noncomplicated appendicitis (Fig. 1). WBC count was 9.42 x109/l with a neutrophil differential of 62.3%. The general surgery service was consulted for the findings. After a full history, physical examination and review of laboratory results and imaging, the patient was taken to laparoscopic appendectomy on the same day of presentation.
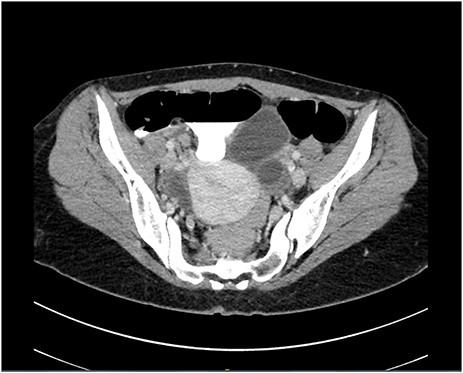
Computed tomography scan in a transverse cut demonstrating an inflamed appendix
Intraoperatively, there were no abnormalities noted at diagnostic laparoscopy. The appendix was identified retrocecally, and the tip was grossly inflamed. The appendix was clipped and resected without any complications. On postoperative day 1, her vital signs were within normal limits, and her abdomen was appropriately tender at incision sites. She was tolerating oral intake with no nausea or vomiting and was discharged home.
The histological examination showed appendiceal diverticulitis, characterized by acutely inflamed pseudodiverticula (herniated mucosa and submucosa through the muscularis propria), associated with peridiverticulitis and periappendicitis, suggesting perforation (Fig. 2a and b).
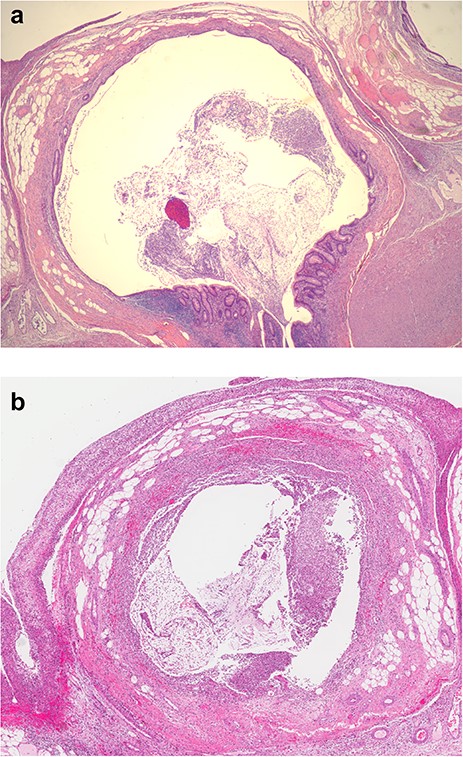
(a) Longitudinal section of appendix shows pseudodiverticulum. (b) Diverticulitis with peridiverticulitis and periappendicitis
On follow up at 2 weeks, she reported mild pain in the left lower quadrant associated with occasional vomiting. This pain persisted at follow-up 2 weeks later, although without nausea or vomiting. There was no alteration in bowel habit. A follow up CT scan was requested, but the patient was lost to follow-up.
DISCUSSION
Diverticulosis of the appendix is classified as congenital and acquired based on the number of appendiceal layers herniating through the normal wall [5]. In the congenital form, mucosa, submucosa and the muscular layer herniate through the wall, while only mucosa with submucosa herniates in the acquired form. The diverticula in this case were acquired, which is the most common form [5]. Risk factors include male gender, age >30 years, Hirschsprung’s disease and cystic fibrosis [6]. According to the appendiceal diverticular disease classification by Phillips et al., this case met the description for microscopic type 1 (primary acute diverticulitis with acute peridiverticulitis) (Table 1) [7].
Appendiceal diverticular disease classification according to Phillips et al. [7]
| Microscopic typologies of appendiceal diverticular disease . | |
|---|---|
| Type 1 | Primary acute diverticulitis, with or without acute peridiverticulitis |
| Type 2 | Acute diverticulitis secondary to acute appendicitis |
| Type 3 | Diverticulum without inflammation |
| Type 4 | Diverticulum with acute appendicitis |
| Type 5 | Chronic peridiverticulitis with acute appendicitis |
| Microscopic typologies of appendiceal diverticular disease . | |
|---|---|
| Type 1 | Primary acute diverticulitis, with or without acute peridiverticulitis |
| Type 2 | Acute diverticulitis secondary to acute appendicitis |
| Type 3 | Diverticulum without inflammation |
| Type 4 | Diverticulum with acute appendicitis |
| Type 5 | Chronic peridiverticulitis with acute appendicitis |
Appendiceal diverticular disease classification according to Phillips et al. [7]
| Microscopic typologies of appendiceal diverticular disease . | |
|---|---|
| Type 1 | Primary acute diverticulitis, with or without acute peridiverticulitis |
| Type 2 | Acute diverticulitis secondary to acute appendicitis |
| Type 3 | Diverticulum without inflammation |
| Type 4 | Diverticulum with acute appendicitis |
| Type 5 | Chronic peridiverticulitis with acute appendicitis |
| Microscopic typologies of appendiceal diverticular disease . | |
|---|---|
| Type 1 | Primary acute diverticulitis, with or without acute peridiverticulitis |
| Type 2 | Acute diverticulitis secondary to acute appendicitis |
| Type 3 | Diverticulum without inflammation |
| Type 4 | Diverticulum with acute appendicitis |
| Type 5 | Chronic peridiverticulitis with acute appendicitis |
Diagnosis is usually made postoperatively at pathology. However, there are reports of cases diagnosed preoperatively on CT scan images [8, 9]. Some studies show that ultrasound can be useful for preoperative diagnosis as well [10]. In this case, the diverticulosis was not radiologically evident and instead was interpreted as acute appendicitis. The histopathology report showed appendiceal diverticulitis and perforation of an inflamed diverticulum with periappendicitis. In addition, the gross appearance of the resected appendix was not suggestive of diverticulosis or any other pathology besides appendicitis. Other cases reported that the gross specimen had evidence of diverticular disease [5].
The CT images in this case were reviewed again with a radiologist and it was confirmed that the features were consistent with acute appendicitis and there was no evidence suggesting the presence of diverticular disease. The reason for the patient’s persistent abdominal pain was not clear. While diverticular disease may be considered, the preoperative imaging did not suggest this. In any case, there is no increased incidence in colonic diverticulosis with appendiceal diverticular disease [2].
CONCLUSION
Appendiceal diverticulosis is an uncommon, but considerable form of appendiceal disease that can present as acute appendicitis and may be associated with a higher risk of perforation and appendiceal neoplasms. Therefore, surgeons should be aware that apparently inflamed appendices may in fact harbor different pathologies and should be followed up accordingly.
Conflict of interest statement
None declared.



