-
PDF
- Split View
-
Views
-
Cite
Cite
Abhay N Dalvi, Mahadeo N Garale, Jayati J Churiwala, Avinash Landge, Sakina Husain, Ajinkya Rewatkar, Pararectal angiomyxoma: a diagnostic dilemma, Journal of Surgical Case Reports, Volume 2019, Issue 12, December 2019, rjz331, https://doi.org/10.1093/jscr/rjz331
Close - Share Icon Share
Abstract
Clinical diagnosis of pararectal masses remains a challenge to this day. Despite the availability of advanced imaging facilities, we often fail to reach a definitive diagnosis and have to resort to surgery. We describe a case of a 60-year-old female with a painless perianal swelling gradually increasing in size for 6 months with spontaneous reduction on assuming a supine position. Clinical examination of this patient was suggestive of a pelvic floor hernia. However, radiological investigations were suggestive of an ischiorectal abscess. In view of lack of radiological corroboration of clinical findings, patient underwent diagnostic laparoscopy which ruled out a hernia. A wide local excision of the mass was performed, which on histopathology with immunohistochemistry examination revealed an aggressive pararectal angiomyxoma.
INTRODUCTION
Aggressive angiomyxoma (AAM) is a benign soft-tissue neoplasm, which has been classified under ‘Tumours of uncertain differentiation’ in the latest WHO classification. This entity is also known as ‘deep aggressive angiomyxoma’. [1] The term aggressive was introduced to emphasize the locally aggressive behaviour along with the high potential for local recurrence. However, it does not infiltrate surrounding organs. This is a rare tumour with ~150 cases reported in the literature.
CASE REPORT
A 60-year-old female presented to the outpatient department of our tertiary care centre with a complain of progressively increasing swelling in the right gluteal region for 6 months associated with dull aching pain radiating to the right lower limb and urinary urgency. The swelling reduced completely and spontaneously on lying down. On clinical examination there was a 5 × 5 cm non-tender swelling in the right pararectal region, which was compressible with positive expansile cough impulse. Per vaginal examination revealed intact vault with swelling felt on the right side. Per rectal and proctoscopic examination was normal. She was a known hypertensive since 25 years on medication with no other comorbidities. Her past surgical history included lower segment caesarean section 25 years back, hysterectomy for uterine fibroids 10 years back followed by ventral hernia repair 9 years back.
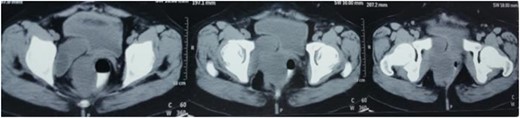
With a differential diagnosis of sciatic hernia or posterolateral perianal hernia in mind the patient was investigated further. A local ultrasound scan was suggestive of an ischiorectal abscess herniating through the sciatic foramen (~130 cc in volume). Since the report did not correlate with the clinical scenario, a contrast-enhanced computerized tomography (CECT) of the abdomen and pelvis was performed which was suggestive of 4.2 × 5.7 × 7.9 cm ischiorectal abscess abutting the rectal wall on the right side with extension down posteriorly and a 3.5 × 4.5 × 3.9 cm cystic lesion posterior to the urinary bladder with a possibility of supralevator extension of the abscess (Fig. 1).
In view of a mismatch between the clinical and radiological findings, it was decided to go ahead with a diagnostic laparoscopy. The findings of laparoscopy were suggestive of an extraperitoneal lesion in the pelvis, ruling out a hernia.
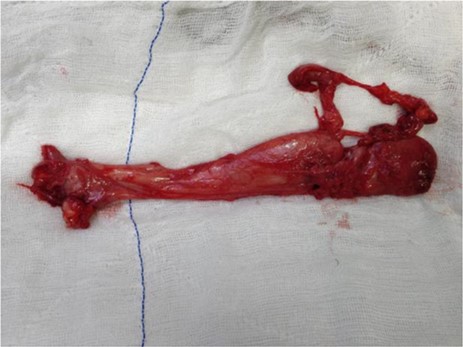
The mass was removed by wide local excision through a pararectal incision maintaining a plane between the rectum and the swelling. The cavity was closed in layers with placement of a corrugated drain (Figs 2 and 3). Final histopathological report was suggestive of a spindle cell tumour and subsequent immunohistochemistry revealed an AAM.

DISCUSSION
AAM is a rare myxoid tumour of mesenchymal origin that arises in the pelvis of women in the reproductive age group but can beseen over a wide age range from 16 to 70 years [2]. Vulva is the most common site of involvement; however, its occurrence in vagina, retroperitoneum, buttock and urinary bladder has also been documented in the literature [2]. AA clinically simulates Bartholin cyst, Gartner duct cyst, vaginal polyp, vaginal cyst, vaginal prolapse, abscess, pelvic floor hernia (as in our case) and other soft-tissue neoplasms [3,4]. Surgery with wide excision is the first line of treatment, although in a few studies wide excision does not lead to a significant lower recurrence rate of AA as compared to incomplete resection.
Adjuvant treatments such as hormone therapy with tamoxifen, raloxifene and gonadotropin-releasing hormone agonists have been used for primary treatment in cases where an extensive surgical procedure will lead to great morbidity and for treatment against tumour recurrence [5–7]. These have been shown to reduce the tumour size and may help to make complete excision feasible in large tumours. Vascular embolization is also used for recurrence [3]. Despite high recurrence rate, the prognosis for patients with AA is generally favourable.
Long-term follow-up is essential in these patients for timely identification of recurrence and prompt resection.



