-
PDF
- Split View
-
Views
-
Cite
Cite
Renee Angela Tabone, Tom DeGreve, Peita Webb, Peter Yuide, Jejuno-jejunal intussusception secondary to diffuse intestinal lipomatosis, Journal of Surgical Case Reports, Volume 2019, Issue 11, November 2019, rjz354, https://doi.org/10.1093/jscr/rjz354
Close - Share Icon Share
Abstract
A 25-year-old man presented to the emergency department with severe abdominal pain and vomiting. He had previously presented 10 days prior with similar symptoms. Computed tomography imaging showed a large jejuno-jejunal intussusception. Multiple intestinal masses were identified intraoperatively with the rare diagnosis of intestinal lipomatosis later confirmed via histopathology. Diagnosis and management of rare surgical pathologies is always challenging. Intussusception should always be considered as a differential diagnosis for abdominal pain in adults, as adult intussusception is typically due to a structural abnormality with majority of cases requiring surgical intervention. Exploratory laparotomy with segmental resection and primary anastomosis proved to be a successful approach in our case, with the patient having an uneventful recovery. Follow-up has consisted of gastrointestinal endoscopy and colonoscopy, which have not demonstrated any further lipomas.
INTRODUCTION
Intussusception is typically a disease of childhood, and its presence in adults is an infrequent clinical entity. Intestinal lipomatosis is a rare pathology, and secondary intussusception is even more uncommon, with only a handful of cases previously documented in the literature. Adult patients often present with intermittent obstructive symptoms, abdominal pain, nausea, rectal bleeding and may have a palpable abdominal mass [1]. Intestinal lipomas are responsible for two-thirds of all enteric intussusceptions [2]; however, they are often solitary opposed to intestinal lipomatosis where the presence of multiple, diffuse and well-circumscribed lipomas exist within the intestinal wall. This care report describes an acute clinical presentation of intussusception secondary to intestinal lipomatosis and subsequent successful surgical intervention.
CASE PRESENTATION
A fit and well 25-year-old man presented to the emergency department with worsening abdominal pain and vomiting. His presentation was on a background of similar intermittent symptoms for the past 12 months. He had previously presented 10 days prior with similar symptoms and was discharged home after a period of observation and improvement in the emergency department; however, he re-presented with a severe episode of pain. He had an unremarkable medical and surgical history. He was a non-smoker and had no significant family history. On physical examination, he was normotensive and afebrile with a heart rate of 90 beats per minute. His abdomen was soft with a tender with a palpable left-sided mass.
Prior to this presentation, the patient had already had an ultrasound examination and routine biochemistry performed, both unremarkable. Computed tomography (CT) imaging was performed at the time of his second presentation which demonstrated a very large intussusception in the left side of his abdomen with proximal jejuno-jejunal involvement, marked enlargement of the intussuscipiens containing the intussusceptum and an enlarged peri-gastric node measuring 17 × 14 × 14mm at the gastric cardia. There were no imaging features suggestive of ischaemic bowel or intestinal lipomatosis (see Figs 1 and 2).

Coronal view of CT imaging demonstrating a very large intussusception on the left side of the abdomen with proximal jejuno-jejunal involvement. Marked enlargement of the intussuscipiens containing the intussusceptum.

Axial section of CT scan demonstrating a rim of contrast material encircling the intussusceptum, representing coating of the opposing bowel walls of the intussusceptum and intussuscipiens, also referred to as the ‘Target Sign’.
The patient was admitted to the hospital and optimised for surgery with intravenous fluid resuscitation and intravenous antibiotics. A midline laparotomy was performed 6 hours after his presentation to the emergency department. Intraoperative findings included an intussusception over 1 metre with the lead point of the intussusception approximately 10 cm from duodenal jejunal flexure. Multiple pathological masses with focal areas of necrosis were present in the wall of small bowel and within the mesentery (see Figs 3 and 4). The intussusception was not reduced as malignancy had not been excluded. The intussusception was resected, and a side-to-side functional end-to-end two-layered hand sewn anastomosis was performed.

Intraoperative photograph demonstrating distended intussuscipiens with intussuscepted segment of jejunum. Multiple polypoid lesions are evident within the small bowel mesentery.
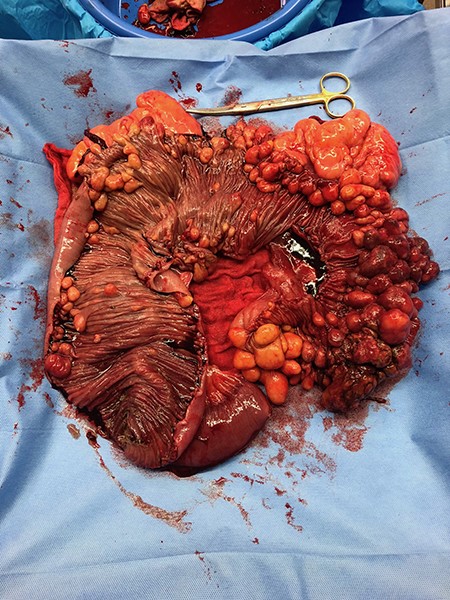
Intraoperative specimen of resected small bowel. Small bowel lumen exposed to show multiple fatty-appearing lesions within small bowel wall.
The resected histology specimen demonstrated numerous polypoid submucosal lipomas and subserosal lipomas (in excess of 100) and associated ischaemic changes. Multiple well-defined polypoid fatty lesions were seen to be arising from the mesenteric surface of the specimen. The largest lesion measured 120 × 60 × 40mm. Lymph nodes demonstrated reactive changes with no evidence of malignancy. The patient recovered well post-operatively without any surgical complications. He was discharged home day 4 post operatively. The patient was followed up for 12 months post operatively. He remained well over this time period, with complete resolution of his previous symptoms. Follow-up endoscopy and colonoscopy 5 months post operatively did not show any remaining lipomas.
DISCUSSION
Intussusception is uncommon in adults with an incidence of two to three cases per 1000000 [3]. Enteric intussusception is the most common form in adults, occurring in 40% of cases. Lipomas are responsible for two-thirds of these cases; however, most of these cases are secondary to a solitary lipoma opposed to intestinal lipomatosis, which is rare and has only been documented in few previous case reports [2, 4–6]. The term intestinal lipomatosis is used to describe diffuse, multiple and circumscribed lipomas within the intestine [7]. Intestinal lipomatosis is a rare disease with an incidence of 0.04–4.5% at autopsy [4]. The pathogenic mechanisms involved in intestinal lipomatosis have not yet been identified; however, several etiological factors have been postulated. These include embryonic displacement of adipose tissue, congenital predisposition, degenerative disease with disturbance of fat metabolism, post-chemotherapeutic fat deposition, chronic inflammatory conditions such as inflammatory bowel disease, infection, hamartomatous syndromes and alcohol consumption [8]. Interestingly, this patient did not have any family or personal history of any such factors, further demonstrating that the pathogenesis of this disease remains poorly understood.
Intestinal lipomatosis is often asymptomatic; however, complications including upper gastrointestinal bleeding, colonic perforation, volvulus and intussusception can occur [2, 4, 6, 9] and are often the first presentation of the condition. There is no consensus in regard to the ideal management approach of intussusception secondary to intestinal lipomatosis. As with other rare surgical conditions, management is difficult to approach due to limited knowledge, limited experience and individual patient factors. In previously published case reports on intussusception secondary to intestinal lipomatosis, a laparotomy and subsequent bowel resection were required [4–6, 10]. One case attempted a 12 hour trial of conservative management [6], another attempted laparoscopic surgery [4]; however, these measures were unsuccessful. A primary anastomosis was successfully performed in all cases. In some previous cases, the intussusception was reduced prior to resection [5]. This is a controversial area due to the risk of potential malignant seeding in cases where the diagnosis of a benign lesion has not been made preoperatively versus a potentially unnecessarily extensive resection. The general consensus within the literature is that reduction should not be attempted if there are signs of irreversible bowel ischaemia or inflammation or when malignancy is suspected [3].
Management of rare surgical pathologies is always challenging. We hope that via sharing our experience and approach, we can assist other surgeons who are faced with a similar patient. As more case reports are published, further advancements towards the surgical management of these rare cases can be established, ultimately leading to improved patient care and outcomes.
References
Author notes
Co-author/immediate supervisor.
- abdominal pain
- computed tomography
- lipoma
- colonoscopy
- adult
- anastomosis, surgical
- differential diagnosis
- emergency service, hospital
- endoscopy, gastrointestinal
- follow-up
- intestines
- intussusception
- lipomatosis
- surgical procedures, operative
- vomiting
- diagnosis
- diagnostic imaging
- jejunum
- laparotomy, exploratory
- histopathology tests



