-
PDF
- Split View
-
Views
-
Cite
Cite
Yuki Matsuoka, Natsuko Kakudo, Michika Fukui, Kenji Kusumoto, Giant plexiform schwannoma in the plantar aspect of the foot: a case report, Journal of Surgical Case Reports, Volume 2019, Issue 11, November 2019, rjz352, https://doi.org/10.1093/jscr/rjz352
Close - Share Icon Share
Abstract
Plexiform schwannoma is a rare Schwann cell tumor that usually occurs in the head and neck. Here, we report a giant plexiform schwannoma (5.5 × 4.0 cm) in the right plantar aspect of the foot. This tumor presented from the dermis to the subcutaneous fat in the plantar aspect, forming a multiocular shape.
INTRODUCTION
Plexiform schwannoma (PS) is an exceedingly rare benign peripheral nerve sheath tumor composed of Schwann cells arranged in a complex, web-like pattern. PS predominantly affects young adults aged 30–40 years, and it commonly occurs as a single, slow-growing, asymptomatic nodule in the dermis or subcutaneous tissue of the head, neck, trunk or upper extremities [1]. Until now, only 15 cases of PS in the foot have been reported [2]. Herein, we describe the case of a 53-year-old female with a large PS in the plantar aspect of her right foot.
CASE REPORT
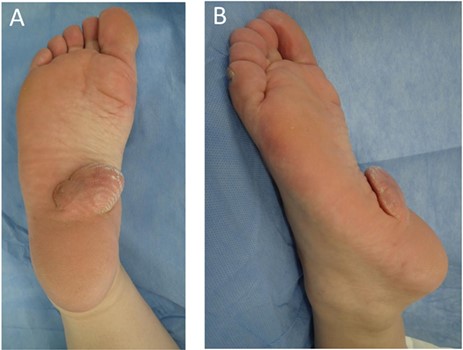
The patient was a 53-year-old female, who had noticed an asymptomatic, skin-colored nodule in her right sole over 30 years prior. The tumor was elastic and soft, measured 5.5 × 4.0 cm and rose up from the plantar aspect of her foot (Fig. 1A and B). Magnetic resonance imaging (MRI) revealed a tumor from the dermis to the subcutaneous fat of the plantar aspect. The tumor was homogeneously isointense relative to the skeletal muscle on T1-weighted images and hyperintense on T2-weighted fat-suppressed images. The tumor contained internal heterogeneous cystic lesions (Fig. 2A–D).
We designed a spindle-shaped incision line on the expanded skin under local anesthesia. We found white tumor tissue spreading from the dermis to the subcutaneous fat of the plantar aspect in a multiocular shape and the bottom of the tumor adhered to the plantar fascia (Fig. 3). The bottom of the tumor was sufficiently separated from the fascia, and the tumor was removed. The base of the tumor was excised from the flap, and the wound was sutured.
Histopathological examination of the tumor by hematoxylin and eosin (H&E) staining revealed multiple lobulated tumors in the dermis and hypodermis. These nodules along the nerve were composed of Schwann cells with uniform spindle cells and nuclear palisading, indicative of Antoni A tissue and Verocay bodies. Myxoid and microcystic areas with a loose meshwork of cells were identified as Antoni B tissue in a small range. No nuclear variant was observed. Myxomatosis and vitrification were found in the center of the specimen (Fig. 4A and B). Microscopically, the tumor was resected completely. According to these clinical and pathological findings, the tumor was formally diagnosed as PS. The wound healed well, and no recurrence of the tumor was noted as of 3 months postoperation.
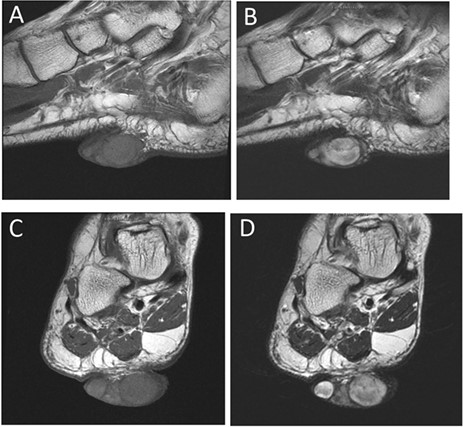
(A) Sagittal view on MRI T1. (B) Sagittal view on MRI T2. (C) Frontal view on MRI T1. (D) Frontal view on MRI T2 (green arrow indicates the tumor).

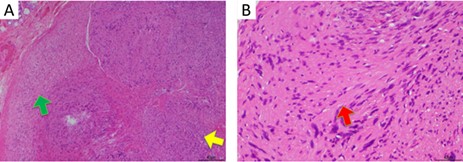
(A) H&E staining at 10× magnification reveals spindle-shaped cells arranged in nuclear palisades, known as Antoni A tissue (indicated by the yellow arrow). A small area was microcystic with a loose meshwork of cells, known as Antoni B tissue (indicated by the green arrow). (B) H&E staining at 40× magnification shows acellular areas located between the regions of nuclear palisading, known as Verocay bodies (indicated by the red arrow).
DISCUSSION
Primary PS was first described by Harkin in 1978 as an extremely rare benign neurogenic tumor, usually affecting the skin or subcutaneous tissue [3]. The plexiform type accounts for 4.3% of all schwannomas, with more than 23% of PS occurring in the head and neck region and 15% occurring cutaneously with a predilection for the head, neck and flexor surfaces of the upper and lower limbs. These tumors present as single, soft-to-rubbery, movable, non-tender and sometimes painful nodules [3]. Trauma may play an etiological role in the formation of these lesions [2]. Most PSs are small, with a maximum diameter of approximately 2 cm and originate from superficial nerves [4].
MRI is a useful tool in the diagnosis of PS; the rims of PS nodules are smooth, and features of the lesions are similar to those of peripheral nerve sheath tumors, including heterogenous hyper- or iso-intensity to subcutaneous fat on T2-weighted MR images. It is reported that multinodular growth patterns in a single lesion and evident cystic degeneration on T2-weighted image are characteristics of PS, which are helpful in the differential diagnosis of these tumors [2]. PS consists of multiple intradermal or subcutaneous nodules composed primarily of cellular Antoni A regions with nuclear palisading and Verocay bodies [2]. In contrast to conventional schwannomas, PS grows in a plexiform pattern consisting of multiple interlacing and interconnecting fascicles and nodules, usually with the Antoni A features of a solitary schwannoma [5], but without Antoni B zones. In this case, the nodules consisted of slender spindle cells with nuclear palisading, and plexiform and spiral arrangements comprised of Verocay bodies.
Malignant transformation of schwannomas is rare, but schwannoma variants, including PS, can be mistaken for more aggressive tumors or suggest the presence of a genetic disease such as neurofibromatosis type 2 (NF2) [5]. Since up to 5% of PS cases may be associated with NF-2, careful intracranial and spinal MRI is necessary to exclude potential NF-2 in young patients [2].
Herein, we have described a rare case of a PS in the plantar aspect of the foot. In contrast to conventional schwannomas, PS is rare, and compared with previous reports, this tumor was located in a rare location. Furthermore, to our knowledge, this is the largest PS reported to date.
ACKNOWLEDGEMENTS
None.
Conflicts of Interest
The authors have no conflicts of interest to disclose.



