-
PDF
- Split View
-
Views
-
Cite
Cite
Anoop Anugraha, Luke D Hughes, Anand Pillai, A novel technique for fabricating antibiotic-coated intramedullary nails using an antibiotic-loaded calcium sulphate hydroxyapatite bio-composite, Cerament-V, Journal of Surgical Case Reports, Volume 2019, Issue 11, November 2019, rjz327, https://doi.org/10.1093/jscr/rjz327
Close - Share Icon Share
Abstract
Deformity correction in the setting of osteomyelitis is a challenge for any orthopaedic surgeon. Principles of management are well described and include staged debridement, stable fixation and a combination of local and systemic antibiotic therapy. An antibiotic-coated nail (ACN) can prove a useful tool—stabilizing bone, whilst allowing for local antibiotic elution. Typically, the surgeon will prepare these implants in the operating room using materials that are routinely at hand. Most frequently, this will involve the use of antibiotic-loaded poly-methyl methacrylate (PMMA). This method of ACN fabrication has several disadvantages. PMMA is non-degradable and can be difficult to remove surgically. There are limitations with regard to antibiotic suitability, antibiotic release as well as toxicity effects. In this case report, we present a novel technique for the preparation of ACNs for use in hindfoot surgery, using a calcium sulphate/hydroxyapatite-based bio-composite—Cerament-V.
INTRODUCTION
Deformity corrections of the hindfoot in diabetic patients with Charcot neuroarthropathy remain a surgical challenge, even in expert hands. If complicated by ulceration and infection, outcomes are even more unpredictable. Infection must first be eliminated. To achieve this, a combination of systemic and local antibiotics may be used.
In 2002, Paley and Herzenberg first described use of antibiotic-coated nails (ACNs) [1] and since then, ACNs have been used extensively to prevent infection in high-risk cases (e.g. open fractures) or to treat established osteomyelitis. ACNs have numerous benefits. They can deliver high doses of antibiotic locally independent of blood supply, whilst also demonstrating very low-serum antibiotic concentrations [2]. With an ability to fill the dead space, they have been demonstrated to prevent bacterial biofilm formation, which can act to protect bacteria against local and systemic antibiotic preparations, making infection very hard to eradicate [3, 4].
Routine use of some ACNs has been limited by their high cost. To circumvent this, many surgeons will fabricate their own nails using materials readily available. Most commonly, this involves the use of antibiotic-loaded poly-methyl methacrylate (PMMA). This bone cement can be moulded about a core, rolled or passed through plastic tubing.
Whilst cheap, the use of PMMA to fabricate nails does have important disadvantages. It is non-degradable, potentially requiring further surgery for its removal. PMMA is incompatible with some antimicrobial agents. The exothermic polymerization reaction generates heat-inactivating heat-liable antibiotics, whilst other antibiotics scavenge free radicals and impair the PMMA polymerization reaction [5]. The elution of antibiotics from PMMA can be highly variable. Studies have demonstrated that less than 10% of the antibiotic is released and that this release is restricted to the first 3–7 days [6, 7].
In this case report, we present an alternative to the use of PMMA for the fabrication of an ACN for use in hindfoot reconstruction. This novel technique involves the use of Cerament, a bio-composite containing calcium sulphate and hydroxyapatite. Cerament-G contains 17.5 mg of gentamycin per ml and Cerament-V contains 66 mg of vancomycin per ml. Both antibiotic-loaded preparations have demonstrated reliable and consistent elution [8, 9] and good success in treating established osteomyelitis reported in the literature [10].
CASE REPORT
A 62-year-old male with a 22-year history of insulin-dependent diabetes and associated neuropathy and retinopathy presented following a fall. He sustained a fifth metatarsal base fracture of his right foot with resultant de-functioning of the peroneus brevis. This led to progressive varus of the forefoot, with subsequent midfoot collapse as a result of Charcot neuroarthropathy (Figs 1 and 2).

Anterior–posterior radiograph of right foot demonstrating fracture at base of fifth metatarsal and forefoot varus.

In May 2015, he had a complex midfoot reconstruction, but his foot continued to drift into varus. This was complicated by an infected ulcer on the lateral aspect of midfoot (Fig. 3). Wound infection progressed to osteomyelitis, and in May 2018, he had a hindfoot reconstruction with fusion of tibiotalar and subtalar joints using a Cerament-V-coated hindfoot nail (Figs 4 and 5).

Clinical photo demonstrating infected ulcer to lateral boarder of right foot.

Anterior–posterior radiograph of right ankle demonstrating tibiotalocalcaneal fusion using a hindfoot nail and screws.
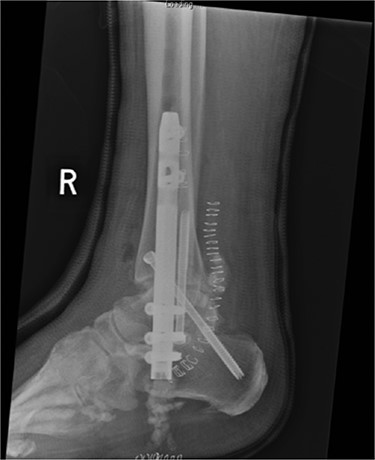
Lateral radiograph of right ankle demonstrating tibiotalocalcaneal fusion using a hindfoot nail and screws.
Preoperatively, radiographs were used to template and to determine the size of the nail. The canal was over reamed by 4 mm: 2 mm of which accommodated for the Cerament mantle, with a further 2 mm to minimise friction during nail insertion. Reamings were sent to microbiology. The canal was washed thoroughly with saline pulsed lavage, gloves were changed and the patient re-draped.
A BIOMET hindfoot nail was attached to its jig and prepared using a single preparation of 10-ml Cerament-V. When in its fluid phase, the Cerament-V was passed through a syringe to cover the nail. The nail was rotated during the setting process such to attain a uniform and smooth surface (Figs 6 and 7). A 14 mm gauge was used to ensure a 2 mm (× 2) thickness of Cerament was achieved. The nail was subsequently inspected such to exclude any defects in the mantle. There was adequate time to ensure that the Cerament had set. Interlocking screw holes were not sited as this may have damaged the cement mould.
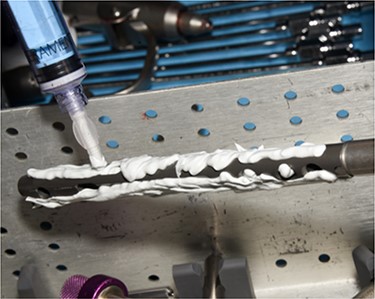
Clinical photo demonstrating syringe application of Cerament-V to hindfoot nail.

Clinical photo demonstrating Cerament mantel around hindfoot nail.
The nail was inserted under guidance from fluoroscopy. Proximal and distal locking was performed through the standard jigs (Fig. 8).

Clinical photo demonstrating hindfoot nail attached to jig, positioned in hindfoot and the citing of locking screws.
DISCUSSION
Cerament is fully bio-absorbable and hence does not require surgical removal. It is both osteoinductive and osteoconductive, remodelled to host bone within 6–12 months [11, 12]. By acting to simulate osteoblasts, Cerament is hypothesised to promote bone union. It is biphasic, meaning that when mixed, it forms an injectable paste, which subsequently hardens. This characteristic allows the easy coating of implants. The setting process is isothermic and is not affected by temperature changes. Antibiotic-loaded preparations demonstrate good elution, with concentrations remaining above the minimum inhibitory concentration for a minimum of 28 days [8, 9]. Proven effective against biofilm formation, Cerament may be used as part of a single-staged treatment protocol for chronic osteomyelitis, eradicating infection and facilitating bony union [10].
The use of a hindfoot nail to achieve tibiotalocalcaneal fusion has several advantages, providing good axial and rotational stability when compared with plates. Usual indications are end-stage ankle and subtalar arthritis, Charcot neuroarthropathy, failed ankle arthroplasty and failed arthrodesis. Active infection is a contraindication. The very fact that intramedullary nails can be an attractive site for bacterial adhesion and biofilm formation [13] leading to persistence of infection is a real concern in cases associated with osteomyelitis or diabetic patients with chronic ulcers. The technique of coating an intramedullary nail with antibiotic-loaded Cerament allows the surgeon to achieve stability and reliable local antibiotic delivery, preventing biofilm formation and treating local osteomyelitis, facilitating successful fusion.
The key concern when using this technique is that the Cerament will debond at the point of nail insertion. This can be avoided by over reaming the canal, ensuring uniform thickness of Cerament and a meticulous technique for insertion.
This is a simple, versatile, cost-effective technique. It does so with a single-stage approach amenable to the resource poor setting.
Conflict of interest statement
None declared.
Funding
The research was supported by funding CERAMENT BONE SUPPORT Inc.



