-
PDF
- Split View
-
Views
-
Cite
Cite
Vassilis G Giannakoulis, Vasiliki Ntella, Andreas Kiriakopoulos, Maria Kostrova, Evangelos Menenakos, Superior mesenteric venous thrombosis as a first manifestation of Antithrombin III deficiency in the postoperative course of laparoscopic sleeve gastrectomy: a case study of 2 patients from 1211 bariatric patients, Journal of Surgical Case Reports, Volume 2019, Issue 11, November 2019, rjz306, https://doi.org/10.1093/jscr/rjz306
Close - Share Icon Share
Abstract
Superior mesenteric venous thrombosis (SMVT) following laparoscopic sleeve gastrectomy (LSG) is a rare, potentially life-threatening complication, which presents either isolated, or as a part of portal/mesenteric/splenic vein thrombosis. Distinction between them possibly confers an important clinical and prognostic value. Antithrombin III (ATIII) deficiency causes an hypercoagulable state which predisposes to SMVT. We report the clinical presentation and treatment of two patients among 1211 LSGs (incidence = 0.165%) that presented with isolated SMVT and ATIII deficiency in an Academic Bariatric Center. Both patients had an unremarkable past medical history; none was smoker or had a previously known thrombophillic condition/thrombotic episode. Mean time of presentation was 15.5 days after LSG. Despite aggressive resuscitative and anticoagulation measures, surgical intervention was deemed necessary. No mortalities were encountered. Coagulation tests revealed ATIII deficiency in both patients.
INTRODUCTION
Laparoscopic sleeve gastrectomy (LSG) has gained an established role in bariatric centers as a weight-loss procedure. A rare, albeit potentially life-threatening complication of LSG is superior mesenteric venous thrombosis (SMVT), either isolated or as a part of portal/mesenteric/splenic vein thrombosis (PMSVT). LSG correlates far more with PMSVT than any other bariatric procedure, with an overall incidence of 0.3% [1]. Distinction between isolated SMVT and PMSVT possibly confers an important clinical and prognostic value [2].
Obesity constitutes a known risk factor for venous thrombosis [3]. LSG procedure poses additional risk due to increased intra-abdominal pressure, reverse Trendelenburg position, sympathetic vasoconstriction, liver retraction and greater curvature skeletonization [1, 4].
Furthermore, hereditary thrombophilia comprises a major risk factor for venous thrombosis. In a recent review of PMSVT cases after bariatric procedures, a thrombophilic condition was found in 46/110 patients [1]. Herein, we present two patients with isolated SMVT after LSG as a first manifestation of Antithrombin III (ATIII) deficiency, in an Academic Bariatric Center.
CASES PRESENTATION
Among 1211 LSGs performed between May 2006–March 2019, two patients presented with isolated SMVT (incidence = 0.165%). Both had unremarkable past medical history and none was smoker or had a previously known thrombophillic condition/thrombotic episode. Upon SMVT diagnosis, intravenous (iv) heparin administration was initiated, in accordance to treatment guidelines [5].
As per protocol, LSG patients receive Low Molecular Weight Heparin (LMWH) as thromboprophylaxis for 7 days postoperatively and they are discharged on the 2nd postoperative day after a routinely performed gastric leak test.
Interestingly, both patients were checked after the episode of SMVT and were found to have ATIII deficiency. One of them exhibited additional V Leiden factor and prothrombin 20210 mutations, whereas the other exhibited protein C deficiency.
Case 1
A 42-year-old male with morbid obesity (BodyMassIndex = 44 kg/m2) underwent LSG. On the 17th postoperative day, he was urgently admitted due to severe abdominal pain/diffuse rebound tenderness. Tachycardia (HR = 140/min) and oliguria (<20 ml/h) were also present. Abdominal Computerized Tomography (CT) demonstrated occlusive thrombus at the main branches of the Superior Mesenteric Vein (SMV), air-fluid levels and small-bowel wall edema with intramural gas (Fig. 1). On exploratory laparotomy, two infarcted, small intestinal segments (totaling 150 cm) were identified. Between them, there was a borderline viable loop. We proceeded to resection of the necrotic bowel and construction of two separate stomas. The patient was eventually discharged on home with total parenteral nutrition feeding and LMWH administration (1.5 mg/kg/d) for 6 months. A successful reversal of the stomas was accomplished 5 months later.
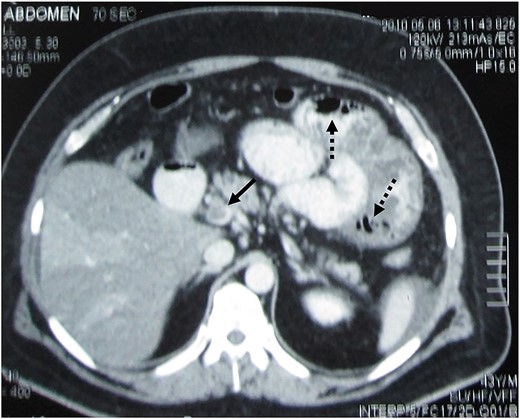
Contrast-enhanced abdominal CT demonstrating SMV thrombosis. Black arrow indicates the thrombus inside the vein, whereas the dotted black arrows indicate gas within the small-bowel wall (pneumatosis intestinalis).
Case 2
A 31-year-old male with morbid obesity (BodyMassIndex = 51 kg/m2) underwent LSG. On the 14th postoperative day, the patient was urgently readmitted due to severe abdominal pain/diffuse tenderness, fever up to 37.8 °C, tachycardia (120/min) and bloody stool passage. An abdominal CT demonstrated thrombosis of the first SMV branches, multiple air fluid levels and an infarcted jejunal segment with edema, wall thickening and intramural bowel gas. On exploratory laparotomy, 120 cm of infarcted jejunum was identified and resected. Intestinal continuity was restored through an end-to-end, hand-sewn anastomosis. Eventually, the patient was discharged in good general condition.
DISCUSSION
SMVT following LSG is a rare complication (incidence: 0,165%). Diagnosis mandates high clinical suspicion; therefore, it may be delayed. Abdominal pain, which is out of proportion to the clinical signs, may prompt further work up. Abdominal CT, which visualizes the thrombus inside the vessel, is the modality of choice for SMVT diagnosis [5].
Regarding isolated SMVT, in a study of 69 patients, the distinction between isolated SMVT and the more extended PMSVT implied important clinical and prognostic differences [2]. Isolated SMVT has been associated with hypercoagulable states and an increased requirement for surgical intervention, contrary to PMSVT, which was commonly attributed to local factors, such as malignancy or splenectomy. Conversely, in a more recent study, isolated SMVT exhibited a more benign course and reduced bowel resection rates [6]. Finally, in a study of 102 patients, no statistically significant difference could be found [7]. These contradictory reports mandate further studies with increased number of patients. Nevertheless, the presence of peritoneal signs, along with CT findings implying bowel necrosis, must be the crucial indicators for surgical intervention [5–7].
In Table 1, we present previous cases of positive thrombophilia testing and PMSVT following LSG. Concerning our study, ATIII is a natural serine protease inhibitor with anticoagulant properties. ATIII deficiency has an estimated prevalence of 1/500–1/5000 in the general population [8]. However, a study reported an increased prevalence of 4/183 in bariatric patients, after routine testing [9]. Clinically, ATIII deficiency mostly manifests as venous thromboembolism and much less commonly as arterial thrombosis [8]. Mesenteric venous thrombosis (MVT) constitutes a rare complication; only 2% of primary MVT is associated with this coagulopathy [10].
Bariatric patients presenting with PMSVT in the postoperative course of LSG.
| Author . | No. of cases . | Management . | Thrombophilia . |
|---|---|---|---|
| Berthet B et al. Obes Surg. 2009 Oct;19:1464-7. | 1 | Heparin | Leiden 2 factor |
| Salinas J et al. Surg Endosc. 2014 Apr;28:1083-9. | 6 | 6/6 Heparin | 4/6 Protein C deficiency 3/6 20210 mutation 2/6 Protein S deficiency |
| Rottenstreich A et al. Surg Obes Relat Dis. 2014 Nov-Dec;10:e57-61 | 1 | LMWH | Lupus-anticoagulant antibodies |
| Roy P et al. Saudi J Obesity 2015; 3: 29-31 | 1 | Patient succumbed. Non-viable bowel on laparotomy. | High homocysteine levels |
| Baba M et al. Case Rep Gastrointest Med. 2015;2015:816914 | 2 | Anticoagulation | 20210 mutation (mother and son) |
| Villagran R et al. Obes Surg. 2016; 26: 2555-2561. | 2 | 2/2 Acenocoumarol | 2/2 Protein C deficiency |
| Parikh M et al. Surg Obes Relat Dis. 2017 Nov;13:1835-1839 | 40 | 36/40 Anticoagulation 2/40 Small-bowel resection 3/40 Endovascular intervention 1/40 Surgical thrombectomy | 25/40 underwent full work-up: 16/25 Elevated factor VIII 12/25 ATIII deficiency 2/25 Protein S deficiency 1/25 Factor V Leiden 1/25 Elevated Cardiolipin IgM 1/25 Protein C deficiency 1/25 Lupus-anticoagulant antibodies 1/25 Plasminogen activator −1 gene polymorphism 1 2/25 No abnormality found |
| Rottenstreich A et al. Surg Obes Relat Dis. 2017 Jan;13:78-84. | 6 | 6/6 Enoxaparin | 2/6 Factor V Leiden 1/6 JAK2 positive 4/6 Elevated factor VIII 1/6 20210 Mutation |
| Copelin E et al. BMJ Case Rep. 2017 May 29;2017. pii: bcr-2016-219167. | 1 | Heparin Blood transfusion Intubation | 20210 Mutation |
| AlSabah SA et al. Obes Surg. 2017 Sep;27:2360-2369 | 2 | Enoxaparin | 1/2 Lupus-anticoagulant antibodies, Anti-phospholipid syndrome 1/2 Protein S deficiency |
| Bain K et al. BMJ Case Rep. 2018 Feb 23;2018. pii: bcr-2017-223937 | 1 | Anticoagulation | ATIII deficiency |
| Our case study | 2 | 2/2 Heparin 2/2 Small-bowel resection | 2/2 ATIII deficiency 1/2 Factor V Leiden + 20210 mutation 1/2 Protein C deficiency |
| Author . | No. of cases . | Management . | Thrombophilia . |
|---|---|---|---|
| Berthet B et al. Obes Surg. 2009 Oct;19:1464-7. | 1 | Heparin | Leiden 2 factor |
| Salinas J et al. Surg Endosc. 2014 Apr;28:1083-9. | 6 | 6/6 Heparin | 4/6 Protein C deficiency 3/6 20210 mutation 2/6 Protein S deficiency |
| Rottenstreich A et al. Surg Obes Relat Dis. 2014 Nov-Dec;10:e57-61 | 1 | LMWH | Lupus-anticoagulant antibodies |
| Roy P et al. Saudi J Obesity 2015; 3: 29-31 | 1 | Patient succumbed. Non-viable bowel on laparotomy. | High homocysteine levels |
| Baba M et al. Case Rep Gastrointest Med. 2015;2015:816914 | 2 | Anticoagulation | 20210 mutation (mother and son) |
| Villagran R et al. Obes Surg. 2016; 26: 2555-2561. | 2 | 2/2 Acenocoumarol | 2/2 Protein C deficiency |
| Parikh M et al. Surg Obes Relat Dis. 2017 Nov;13:1835-1839 | 40 | 36/40 Anticoagulation 2/40 Small-bowel resection 3/40 Endovascular intervention 1/40 Surgical thrombectomy | 25/40 underwent full work-up: 16/25 Elevated factor VIII 12/25 ATIII deficiency 2/25 Protein S deficiency 1/25 Factor V Leiden 1/25 Elevated Cardiolipin IgM 1/25 Protein C deficiency 1/25 Lupus-anticoagulant antibodies 1/25 Plasminogen activator −1 gene polymorphism 1 2/25 No abnormality found |
| Rottenstreich A et al. Surg Obes Relat Dis. 2017 Jan;13:78-84. | 6 | 6/6 Enoxaparin | 2/6 Factor V Leiden 1/6 JAK2 positive 4/6 Elevated factor VIII 1/6 20210 Mutation |
| Copelin E et al. BMJ Case Rep. 2017 May 29;2017. pii: bcr-2016-219167. | 1 | Heparin Blood transfusion Intubation | 20210 Mutation |
| AlSabah SA et al. Obes Surg. 2017 Sep;27:2360-2369 | 2 | Enoxaparin | 1/2 Lupus-anticoagulant antibodies, Anti-phospholipid syndrome 1/2 Protein S deficiency |
| Bain K et al. BMJ Case Rep. 2018 Feb 23;2018. pii: bcr-2017-223937 | 1 | Anticoagulation | ATIII deficiency |
| Our case study | 2 | 2/2 Heparin 2/2 Small-bowel resection | 2/2 ATIII deficiency 1/2 Factor V Leiden + 20210 mutation 1/2 Protein C deficiency |
Only cases with positive thrombophilic testing were included.
Bariatric patients presenting with PMSVT in the postoperative course of LSG.
| Author . | No. of cases . | Management . | Thrombophilia . |
|---|---|---|---|
| Berthet B et al. Obes Surg. 2009 Oct;19:1464-7. | 1 | Heparin | Leiden 2 factor |
| Salinas J et al. Surg Endosc. 2014 Apr;28:1083-9. | 6 | 6/6 Heparin | 4/6 Protein C deficiency 3/6 20210 mutation 2/6 Protein S deficiency |
| Rottenstreich A et al. Surg Obes Relat Dis. 2014 Nov-Dec;10:e57-61 | 1 | LMWH | Lupus-anticoagulant antibodies |
| Roy P et al. Saudi J Obesity 2015; 3: 29-31 | 1 | Patient succumbed. Non-viable bowel on laparotomy. | High homocysteine levels |
| Baba M et al. Case Rep Gastrointest Med. 2015;2015:816914 | 2 | Anticoagulation | 20210 mutation (mother and son) |
| Villagran R et al. Obes Surg. 2016; 26: 2555-2561. | 2 | 2/2 Acenocoumarol | 2/2 Protein C deficiency |
| Parikh M et al. Surg Obes Relat Dis. 2017 Nov;13:1835-1839 | 40 | 36/40 Anticoagulation 2/40 Small-bowel resection 3/40 Endovascular intervention 1/40 Surgical thrombectomy | 25/40 underwent full work-up: 16/25 Elevated factor VIII 12/25 ATIII deficiency 2/25 Protein S deficiency 1/25 Factor V Leiden 1/25 Elevated Cardiolipin IgM 1/25 Protein C deficiency 1/25 Lupus-anticoagulant antibodies 1/25 Plasminogen activator −1 gene polymorphism 1 2/25 No abnormality found |
| Rottenstreich A et al. Surg Obes Relat Dis. 2017 Jan;13:78-84. | 6 | 6/6 Enoxaparin | 2/6 Factor V Leiden 1/6 JAK2 positive 4/6 Elevated factor VIII 1/6 20210 Mutation |
| Copelin E et al. BMJ Case Rep. 2017 May 29;2017. pii: bcr-2016-219167. | 1 | Heparin Blood transfusion Intubation | 20210 Mutation |
| AlSabah SA et al. Obes Surg. 2017 Sep;27:2360-2369 | 2 | Enoxaparin | 1/2 Lupus-anticoagulant antibodies, Anti-phospholipid syndrome 1/2 Protein S deficiency |
| Bain K et al. BMJ Case Rep. 2018 Feb 23;2018. pii: bcr-2017-223937 | 1 | Anticoagulation | ATIII deficiency |
| Our case study | 2 | 2/2 Heparin 2/2 Small-bowel resection | 2/2 ATIII deficiency 1/2 Factor V Leiden + 20210 mutation 1/2 Protein C deficiency |
| Author . | No. of cases . | Management . | Thrombophilia . |
|---|---|---|---|
| Berthet B et al. Obes Surg. 2009 Oct;19:1464-7. | 1 | Heparin | Leiden 2 factor |
| Salinas J et al. Surg Endosc. 2014 Apr;28:1083-9. | 6 | 6/6 Heparin | 4/6 Protein C deficiency 3/6 20210 mutation 2/6 Protein S deficiency |
| Rottenstreich A et al. Surg Obes Relat Dis. 2014 Nov-Dec;10:e57-61 | 1 | LMWH | Lupus-anticoagulant antibodies |
| Roy P et al. Saudi J Obesity 2015; 3: 29-31 | 1 | Patient succumbed. Non-viable bowel on laparotomy. | High homocysteine levels |
| Baba M et al. Case Rep Gastrointest Med. 2015;2015:816914 | 2 | Anticoagulation | 20210 mutation (mother and son) |
| Villagran R et al. Obes Surg. 2016; 26: 2555-2561. | 2 | 2/2 Acenocoumarol | 2/2 Protein C deficiency |
| Parikh M et al. Surg Obes Relat Dis. 2017 Nov;13:1835-1839 | 40 | 36/40 Anticoagulation 2/40 Small-bowel resection 3/40 Endovascular intervention 1/40 Surgical thrombectomy | 25/40 underwent full work-up: 16/25 Elevated factor VIII 12/25 ATIII deficiency 2/25 Protein S deficiency 1/25 Factor V Leiden 1/25 Elevated Cardiolipin IgM 1/25 Protein C deficiency 1/25 Lupus-anticoagulant antibodies 1/25 Plasminogen activator −1 gene polymorphism 1 2/25 No abnormality found |
| Rottenstreich A et al. Surg Obes Relat Dis. 2017 Jan;13:78-84. | 6 | 6/6 Enoxaparin | 2/6 Factor V Leiden 1/6 JAK2 positive 4/6 Elevated factor VIII 1/6 20210 Mutation |
| Copelin E et al. BMJ Case Rep. 2017 May 29;2017. pii: bcr-2016-219167. | 1 | Heparin Blood transfusion Intubation | 20210 Mutation |
| AlSabah SA et al. Obes Surg. 2017 Sep;27:2360-2369 | 2 | Enoxaparin | 1/2 Lupus-anticoagulant antibodies, Anti-phospholipid syndrome 1/2 Protein S deficiency |
| Bain K et al. BMJ Case Rep. 2018 Feb 23;2018. pii: bcr-2017-223937 | 1 | Anticoagulation | ATIII deficiency |
| Our case study | 2 | 2/2 Heparin 2/2 Small-bowel resection | 2/2 ATIII deficiency 1/2 Factor V Leiden + 20210 mutation 1/2 Protein C deficiency |
Only cases with positive thrombophilic testing were included.
In our cases, thromboprophylaxis and an initial, non-surgical treatment attempt proved insufficiency, due to heparin resistance. Heparin resistance describes an inadequate response to heparin administration, primarily due to low levels of ATIII [8]. Since ATIII deficiency screening prior to LSG is not recommended, heparin resistance could not be suspected preoperatively in our cases. In conclusion, isolated SMVT following LSG is an extremely rare complication, associated with life-threatening consequences. Its occurrence appears to be multifactorial and high clinical suspicion is required. Additionally, the presence of ATIII deficiency may confer an important clinical and prognostic value.
Study Funding
The study received no funding.
Conflicts of Interest
None to declare.
REFERENCES
- anticoagulation
- thrombophilia
- antithrombin iii deficiency
- blood coagulation tests
- mesentery
- resuscitation
- surgical procedures, operative
- antithrombin iii
- medical history
- mortality
- patient prognosis
- splenic vein thrombosis
- thrombus
- thrombosis of mesenteric vein
- bariatric surgery
- sleeve gastrectomy, laparoscopic
- smokers



