-
PDF
- Split View
-
Views
-
Cite
Cite
Sawsan F Almarzouq, Mohammed A Almarghoub, Obaid Almeshal, Primary actinomycosis of the big toe: a case report and literature review, Journal of Surgical Case Reports, Volume 2019, Issue 11, November 2019, rjz292, https://doi.org/10.1093/jscr/rjz292
Close - Share Icon Share
Abstract
Actinomyces are Gram-positive branching bacteria that are part of the human gastrointestinal microflora. These organisms can cause actinomycosis, which is a slowly progressive suppurative infection involving the cervicofacial region. Primary involvement of extremities is very rare. Here, we present primary actinomycosis of the lower extremity and a review of related literature. A 35-year-old female from Al-Kharj City (agricultural area) presented to our plastic surgery clinic with complaints of a large mass on the left big toe that caused embarrassment and difficulty in wearing footwear. The patient underwent wide local excision and coverage of the big toe defect with Kutler bilateral V-Y advancement flaps. A high index of suspicion is required to diagnose actinomycosis in subacute or chronic inflammatory soft tissue lesions. Proper surgical intervention and antimicrobial are essential to treat the disease. We conclude that a high index of suspicion is required to diagnose actinomycosis in subacute or chronic inflammatory soft tissue lesions.
INTRODUCTION
Actinomycosis is caused by Gram-positive branching bacteria of the genus actinomycosis that live within the human microflora in the oral and gastrointestinal tract. This infection has a slowly progressive, suppurative indolent course and is mostly detected in the cervicofacial (55%), abdominopelvic (20%) and pulmothoracic (15%) regions [1]. Extremity involvement is usually secondary to the local extension or hematogenous spread, and primary limb involvement is very rare [2]. Moreover, chronic non-healing wound in the extremity associated with granule-like material is associated with a high suspicion of actinomycosis infection [3]. Primary involvement of the lower extremity was reported before in the literature [4, 5]. Here, we report a patient with primary cutaneous actinomycosis occurring in the left big toe that was treated by wide local excision and coverage of the defect with Kutler bilateral V-Y advancement flaps [6].
CASE PRESENTATION
A 34-year-old previously healthy female presented with a mass on the left big toe that caused embarrassment and difficulty in wearing footwear. The mass was first noticed three years ago and has since started to grow in size. There was no associated discharge, skin changes or other masses elsewhere. The patient had no history of trauma, contact with an animal, and animal or human bite. She lived in an agricultural area and indulged in barefoot walking. The patient had neither history of any systemic illness or weight loss, fever, or easily fatigability nor any significant family history. However, the patient had a similar mass at the same site that was treated surgically 15 years ago and failed to provide any information regarding its diagnosis.
Upon examination, the patient was conscious, alert and oriented and not pale, jaundiced or cyanosed. Her vitals were normal, and the liver, spleen and lymph nodes were not palpable. Cardiovascular system, respiratory system and the central nervous system showed no abnormalities. Left big toe examination revealed 2 × 1 × 1 cm mass at the distal end. There were no changes in the overlying skin or the nail and no surrounding cellulitis. The distal neurovascular examination revealed normal findings. There was no palpable inguinal lymphadenopathy.
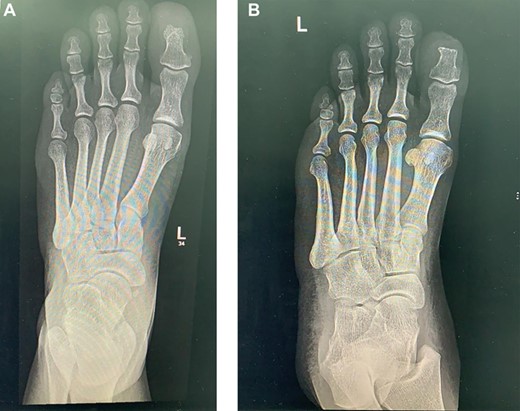
The laboratory data included a white blood cell count of 6000/μl, hemoglobin of 10.5 g/dl, platelet count of 233 × 10/μl, blood glucose 121 mg/dl, blood urine nitrogen 46 mg/dl, serum creatinine 69 mg/dl, sodium 138 mmol/L, potassium 3.8 mmol/L, serum albumin 3.4 g/dl, erythrocyte sedimentation rate 73 mm/h, and C-reactive protein 15.6 mg/dl. The X-ray of lower extremity revealed no significant abnormality (Fig. 1).
Incisional biopsy showed chronic inflammation with scattered granulomas mixed with neutrophils and actinomycetes.
MRI showed a 2-cm soft tissue focus at the tip and plantar aspect of big toe closely adherent to the tuft of distal phalanx but with no evidence of bony destruction (Fig. 2).

Pre-excision MRI for the right foot showing a 2-cm soft tissue focus at the tip and plantar aspect of big toe closely adherent to the tuft of distal phalanx but with no evidence of bony destruction.
The mass was shaved off the bone with wide local excision, and the resultant defect was covered with Kutler bilateral V-Y advancement flaps (Fig. 3).

One-week post excision and coverage with Kutler bilateral V-Y advancement flaps.
Final histopathology showed reactive epidermis with subepidermal multiple colonies of filamentous organisms with extensive mixed inflammatory reaction consistent with actinomycosis.
The patient was then referred to the infectious disease team, and a 6-week course of clindamycin was started to eradicate the infection. Follow up after 19 months shows no recurrence (Figs 4 and 5).

19 months post excision and coverage with Kutler bilateral V-Y advancement flaps with no evidence of recurrence.

Left foot X-ray 19 months post excision and coverage with Kutler bilateral V-Y advancement flaps no evidence of recurrence.
DISCUSSION
Actinomyces are Gram-positive, non-spore forming, anaerobic bacillus bacteria that cause actinomycosis. These bacteria are found normally as part of the human flora in the oral and gastrointestinal tract [1].
Cutaneous infections are caused by hematogenous spread or traumatic injury. These infections mostly affect the cervicofacial (55%), abdominopelvic (20%) and pulmothoracic regions (15%) [1]. Actinomycosis of the extremity is rare. Around 50 cases of primary limb involvement have been reported in the literature [2, 7–10]. Specific involvement of the lower limb has been published before [4, 5]. However, it has not been described in the Middle East. A high index of suspicion in chronic non-healing skin lesion is recommended to diagnose this infection [3]. Clinically, the disease course is indolent with any of the following: nodular lesion, subcutaneous abscess and mass mimicking tumor as presented in our case [11].
Most reported cases have a preceding history of trauma. The infection can spread from the skin to the subcutaneous tissue, muscles and bone [2, 11].
Sulfur granules are the hallmark of actinomycosis. To confirm the diagnosis, the organism can be isolated from these granules in histopathological samples. However, the samples usually contain few granules that make the diagnosis difficult [11]. In this case, incisional biopsy showing Actinomyces can raise the concern of actinomycosis infection. The diagnosis can be confirmed after the excision of the whole mass.
Treatment of actinomycosis consists of surgical intervention and appropriate antimicrobial therapy [3]. Penicillin is the drug of choice for treating the infection. Initially, it is given parenterally in high doses and then orally for a prolonged duration of ~12 months depending on the disease severity. In penicillin-allergic patients, tetracycline, erythromycin and clindamycin can be considered as suitable drug alternatives [11, 12]. In our case, the patient was presented with soft tissue mass in its clinical features and X-ray findings. This is an uncommon clinical presentation for actinomycosis, which could be misdiagnosed. Combining clinical approach and histological features is indispensable to reach the accurate diagnosis.
FINANCIAL DISCLOSURE
The authors have no financial interest to declare in relation to the content of this article.
CONFLICT OF INTEREST
None declared.
AUTHORS PARTICIPATION
Obaid Almeshal operated on the patient and wrote the abstract and edited the manuscript. Sawsan F. Almarzouq and Mohammed A. Almarghoub wrote the manuscript, took the photographs followed the patient.
INFORMED CONSENT
Informed consent was obtained from the participant included in this study.
ETHICAL APPROVAL
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
REFERENCES
- actinobacteria
- actinomycosis
- limb
- gram-positive bacteria
- gram-positive bacterial infections
- gram-positive cocci
- gram-positive rods
- hallux
- suppuration
- surgical procedures, operative
- bacteria
- leg
- plastic surgery specialty
- plastic surgery procedures
- antimicrobials
- v-y advancement flap
- soft tissue
- wide local excision
- embarrassment



