-
PDF
- Split View
-
Views
-
Cite
Cite
Adam O’Connor, Sanjay Furtado, Septic arthritis of the manubriosternal joint presenting as a chest-wall swelling in an immunocompetent patient, Journal of Surgical Case Reports, Volume 2019, Issue 11, November 2019, rjz261, https://doi.org/10.1093/jscr/rjz261
Close - Share Icon Share
Abstract
Septic arthritis of the manubriosternal joint is a rare pathology, often mistaken for other disease processes given its location and chest pain symptoms. We present a case of a 58-year-old man presenting with a dull ache in his chest after returning from a holiday. Initially under the care of the physicians locally, he was investigated for respiratory and cardiac causes of chest pain with no findings. Eventually, a lump was noted on examination of the chest prompting further imaging, which confirmed a diagnosis of manubriosternal septic arthritis. He was discussed and referred to tertiary cardiothoracics, who recommended conservative treatment with 6 weeks of antibiotics. To date, there has been a good recovery. We present this case alongside a discussion of the limited literature, in particular highlighting how difficult a diagnosis it is to make but one that surgeons and medics alike should be aware of.
INTRODUCTION
Septic arthritis of the manubriosternal joint is a rare pathology with only nine cases identified in the literature. Being so rare, it is often mistaken for another disease process such as abscess and often presents with symptoms of chest pain, which undergoes extensive diagnostic work up to exclude more immediate problems such as cardiac or pulmonary causes of chest pain. The chest-wall swelling can be easy to miss and sometimes not even noticed by the patient, as in our case initially. We present the case of a 58-year-old man presenting initially with chest pain, but no significant past medical history. Ultimately, his diagnosis emerged as septic arthritis of the manubriosternal joint, which we attempt to explore in this article.
CASE REPORT
A previously well 58-year-old man initially presented with chest pain having returned from holiday and was admitted under the care of the physicians. He described a dull ache across the chest, not pleuritic in nature and with no associated dyspnoea, cough or haemoptysis. There was no history of trauma. Physical examination at that time was unremarkable and the patient did not report any swellings of the chest wall. Blood results revealed a C Reactive protein (CRP), of 88 mg/l, a d-dimer of 2137 ng/ml, liver function tests (LFT) derangement but a normal Full blood count (FBC). Given the d-dimer, computed tomography pulmonary angiography (CTPA) was performed to exclude pulmonary embolism. This showed no Pulmonary embolism (PE), pneumothorax or pneumonia. Instead, it showed subcutaneous tissue stranding in the midline anterior to the manubrium and upper sternum with soft tissue thickening inseparable from the medial pectoral muscles. On further examination of the chest, there was a tender, prominent sternum with mild erythema but no warmth. The patient was discharged from the medical team with ibuprofen gel and advised to seek medical attention should he develop any signs of infection.
He then presented 3 weeks later referred by his general practitioner (GP) to the surgical hot clinic with worsening swellings of the sternum and discharge from the inferior aspect of the sternum. He had been given oral flucloxacillin by the GP, but was clinically well and not septic. Physical observations were within normal limits. On examination, there was a 3 × 3 cm swelling overlying the body of the sternum with discharge. Superior to that was another diffuse inflammatory swelling. Blood tests revealed CRP of 86, his LFTs had returned to normal and FBC was normal. Options were considered as to whether to drain under lupus anticoagulant, but given the recent computed tomogramphy (CT) chest showing possible pectoral involvement, the decision was made to admit to hospital for incision and drainage under GA. He was consented as such and admitted. He was then reviewed the next day by the on call consultant surgeon, who felt given the prolonged history of the swelling that an abscess was unlikely. Magnetic resonance imaging (MRI) of the sternum was, therefore, recommended by the radiologists to further characterize the lesion (Fig. 1a–c). MRI of the area revealed fluid within the manubriosternal joint with erosion of the articular margins. A fluid collection 65 × 7 mm was presented within the right pectoralis major, along with a small collection in the medial aspect of left pectoralis major. Also present was surrounding soft tissue thickening and oedema with marrow oedema of the upper body of sternum and manubriosternal joint. No abnormality was demonstrated in the underlying mediastinum. The MRI concluded that this was septic arthritis of the manubriosternal joint with bony erosion and underlying osteomyelitis.
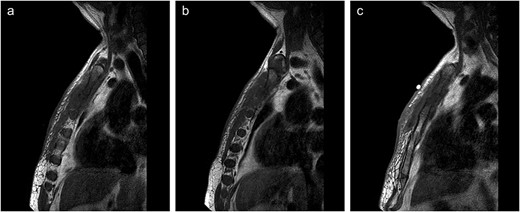
(a–c) Lateral views of sternal MRI showing varying degrees of inflammation and septic arthritis of manubriosternal joint.
He was subsequently commenced on intravenous flucloxicillin and discussed with the cardiothoracic regional centre on call, who advised conservative management with antibiotics for 6 weeks. This was agreed with the local microbiologists, who advocated metronidazole and clindamycin therapy for the same period of time. To date, his recovery has been excellent and he is progressing well.
DISCUSSION
Septic arthritis of the manubriosternal joint in an immunocompetent patient is rare [1]. Most commonly, it is related to intravenous drug abuse via the transmission of infection in the upper limbs with axillary and subclavian phlebitis but other primary sources such as distant septic arthritis, GI infection and cellulitis have been implicated [2]. Both acute septic responses and more indolent, subacute courses as in our case have been described in the literature with one particular case demonstrating a course of 18 months. [3, 4]. Parity of septic arthritis in the manubriosternal joint is in part due to its anatomy. Being a symphysis, despite case reports of infection of the pubic symphysis, the rates of septic arthritis are massively lower than in synovial joints [5]. Coagulase positive staph aureus is the primary pathogen in 60% of the cases with some suggestions also of the importance in the disease of salmonella and pseudomonas [1]. No positive cultures were identified in our patient.
In terms of diagnosis, the disease process may or may not be present on sternal radiographs [6]. The presence of soft tissue and joint destruction on CT or MRI scans demonstrates a later stage of the disease process [7]. The small incidence of septic arthritis in this location makes the diagnosis challenging, and there is often misdiagnosis of the case as in our case, where more acute, medically orientated diagnosis were considered foremost [1]. Regarding management, in early stages of the disease, intravenous antibiotics are the mainstay with surgical washout indicated in upwards of 60% of cases [4]. Post-washout, large defects in the pectoral area may be treated with pectoralis flap; however, this depends upon factors such as patient’s age, occupation and general functional status [8].
Conflict of interest statement
None declared.
Funding
None.
Patient Consent
Obtained.



