-
PDF
- Split View
-
Views
-
Cite
Cite
S J Dancer, S G Macpherson, A C de Beaux, Protracted diagnosis of ACNES: a costly exercise, Journal of Surgical Case Reports, Volume 2018, Issue 9, September 2018, rjy230, https://doi.org/10.1093/jscr/rjy230
Close - Share Icon Share
Abstract
This case report summarizes the course of events leading to diagnosis and eventual repair of anterior cutaneous nerve entrapment syndrome (ACNES) in a 58-year-old female. The time period elapsing from initial symptoms to final operative repair was 9 months. The diagnosis was missed by both medical and surgical specialists despite multiple outpatient appointments, investigative procedures and a battery of laboratory tests. The diagnosis of ACNES was first considered when reviewed by a hernia surgeon and subsequently confirmed following open exploration of the anterior abdominal wall. The nerve was released and pain symptoms resolved. Access to the NHS Scotland ISD register permitted an economic analysis of the diagnostic services utilized for this patient and these totalled nearly £11 500. At a time when the NHS is focused on cost effectiveness, this particular sequence of investigations illustrates a protracted and costly diagnostic pathway.
INTRODUCTION
Anterior cutaneous nerve entrapment syndrome (ACNES) is due to irritation of intercostal thoracic nerve roots passing through the abdominal fascia (Fig. 1) [1, 2]. The abdominal cutaneous nerve runs anterior to the transversus abdominis muscle for most of its course before the anterior branch pierces the rectus fascia to lie anterior to rectus abdominis muscle. The syndrome is caused by entrapment of this branch as it makes its way through the anterior rectus muscle fascia at almost 90° [3]. Compression may be due to herniation of the fat pad that normally protects the nerve within the fibrous canal [4]. The patient is able to pinpoint the pain with one finger at the exact site at which the nerve is compressed and this is an important feature of the syndrome. Another diagnostic feature is a positive Carnett’s sign, which is useful for confirming whether pain originates from abdominal viscera or from the abdominal wall [5, 6]. The incidence of ACNES is thought to be 10–30% of patients with chronic abdominal wall pain [7].
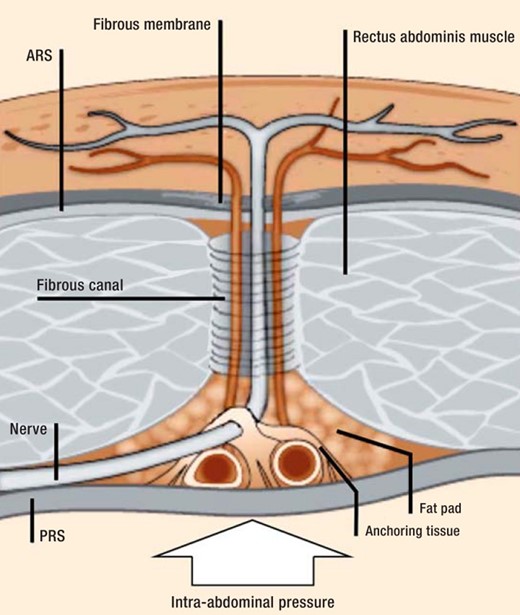
The nerves of the anterior abdominal wall and their double right-angle course at the lateral edge of rectus abdominis muscle.
CASE REPORT
The patient is a 58-year-old female musician. She presented to the GP in September 2017 complaining of mild but persistent abdominal pain in the left iliac fossa. The pain resembled tooth-ache and increased with movement. She denied any other signs or symptoms, other than a single episode of perineal bleeding. The GP referred the patient for urgent vaginal ultrasound given a family history of ca ovary. This was normal, along with a series of blood tests and cancer markers. The patient then underwent CT scan with contrast, which showed a subserosal tumour at the left upper uterine margin accompanied by free fluid. A consultant gynaecologist and consultant surgeon undertook dual exploratory laparoscopy and hysteroscopy in mid-November 2016. They located the tumour (fibroid) and found an incidental liver haemangioma. All biopsies were negative.
The pain increased and began to radiate toward the left inguinal region. Since the patient had previously experienced disc prolapse with surgical repair, she underwent MRI scanning to exclude discitis and/or psoas abscess. As this was unremarkable, she then had a liver ultrasound in January 2018, which showed mild fatty liver. Subsequent gastroenterology referral diagnosed hypothyroidism and stress and she was offered laxatives and anti-depressants [6].
The patient could pinpoint an exquisitely tender site below and lateral to the umbilicus. This was duplicated when she was supine, provided the head was raised [5]. Increasing pain was related to playing the saxophone, occurring shortly after intensive practice or performance. A hernia was suspected and the GP referred the patient for abdominal ultrasound performed standing and supine, with coughing and forced Valsalva. This showed a small (<1 cm) hypoechoic cyst protruding through a deficit between left external oblique and transversus abdominis, suggesting left lateral ventral (Spigelian) hernia [8]. The patient underwent laparoscopy in February 2018.
The exact point of tenderness was incorrectly marked prior to surgery (Fig. 2), making it impossible for the surgeon to locate any muscle deficit at operation. The patient had two further MRI scans, both of which were indeterminate and she was then referred to a hernia surgeon. The possibility of ACNES was undoubtedly made easier by previous cross-sectional imaging and laparoscopy demonstrating no obvious intra-abdominal pathology or abdominal wall hernia. Nevertheless, there is little intra-abdominal pathology that presents with localized, almost point tenderness to the anterior abdominal wall. The final diagnosis was made following an exploration of the anterior abdominal wall. The exact point of maximum tenderness was carefully marked before surgery with the patient in a supine position. A small incision was made at the marked point, and at the level of the fascia, the anterior cutaneous nerve was evident exiting the fascia. The exit site was enlarged with a pair of forceps, and a very small lipoma became evident lying beneath the fascia, which was removed. As previous imaging had suggested a small Spigelian hernia, the lateral muscles at the same level were explored but no hernia was identified.

Photograph of patient’s left lower abdomen showing point of maximal tenderness (X) and indelible pen circle marked before failed surgical endoscopy. Photo: Donna D.
All investigative procedures and tests for this patient were costed according to NHS Scotland National Statistical Data (http://www.isdscotland.org/Health-Topics/Finance/Costs/). Itemized and total costs for the patient are shown in Table 1. There were notable differences between the costs for duplicate investigations and consultant appointments between three Scottish Health boards. The most expensive procedures were inpatient operations, with day surgery procedures less than half the cost. The total cost of all procedures and tests over the 9-month period was £11 482.74.
Itemized and total costs of investigative procedures for a patient with ACNES
| Procedure . | Health board . | Cost per item (£)* . | No. of items . | Total cost (£) . |
|---|---|---|---|---|
| Hysteroscopy (day surgery) | NHS Lanarkshire | £923.00 | 1 | £923.00 |
| Endoscopy (day surgery) | NHS Lanarkshire | £923.00 | 1 | £923.00 |
| Endoscopy (in-patient) 6 nights | Greater Glasgow & Clyde | £2625.00 | 1 | £2625.00 |
| Open exploration (in-patient) I night | NHS Lothian | £3511.00 | 1 | £3511.00 |
| MRI | NHS Lanarkshire | £188.92 | 1 | £188.92 |
| CT scan | NHS Lanarkshire | £83.74 | 1 | £83.74 |
| Abdominal ultrasound | NHS Lanarkshire | £43.08 | 1 | £43.08 |
| Vaginal ultrasound | Greater Glasgow & Clyde | £55.35 | 1 | £55.35 |
| Abdominal ultrasound | Greater Glasgow & Clyde | £55.35 | 1 | £55.35 |
| MRI | Greater Glasgow & Clyde | £214.16 | 2 | £428.32 |
| Consultant appointment | NHS Lanarkshire | £149.00 | 3 | £447.00 |
| Consultant appointment | Greater Glasgow & Clyde | £204.00 | 4 | £816.00 |
| Consultant appointment | NHS Lothian | £157.00 | 2 | £314.00 |
| GP appointment | Greater Glasgow & Clyde | £100.00 | 5 | £500.00 |
| A&E attendance | Greater Glasgow & Clyde | £135.00 | 2 | £270.00 |
| Haematology | Greater Glasgow & Clyde | £5.27 | 7 | £36.89 |
| Clinical chemistry | Greater Glasgow & Clyde | £0.91 | 10 | £9.10 |
| Urinalysis | Greater Glasgow & Clyde | £16.32 | 1 | £16.32 |
| Haematology | NHS Lanarkshire | £5.37 | 6 | £32.22 |
| Clinical chemistry | NHS Lanarkshire | £0.80 | 10 | £8.00 |
| Urinalysis | NHS Lanarkshire | £10.46 | 3 | £31.38 |
| Pathology | NHS Lanarkshire | £27.77 | 3 | £83.31 |
| Cancer markers | NHS Lanarkshire | £40.88 | 2 | £81.76 |
| Total | £11 482.74 |
| Procedure . | Health board . | Cost per item (£)* . | No. of items . | Total cost (£) . |
|---|---|---|---|---|
| Hysteroscopy (day surgery) | NHS Lanarkshire | £923.00 | 1 | £923.00 |
| Endoscopy (day surgery) | NHS Lanarkshire | £923.00 | 1 | £923.00 |
| Endoscopy (in-patient) 6 nights | Greater Glasgow & Clyde | £2625.00 | 1 | £2625.00 |
| Open exploration (in-patient) I night | NHS Lothian | £3511.00 | 1 | £3511.00 |
| MRI | NHS Lanarkshire | £188.92 | 1 | £188.92 |
| CT scan | NHS Lanarkshire | £83.74 | 1 | £83.74 |
| Abdominal ultrasound | NHS Lanarkshire | £43.08 | 1 | £43.08 |
| Vaginal ultrasound | Greater Glasgow & Clyde | £55.35 | 1 | £55.35 |
| Abdominal ultrasound | Greater Glasgow & Clyde | £55.35 | 1 | £55.35 |
| MRI | Greater Glasgow & Clyde | £214.16 | 2 | £428.32 |
| Consultant appointment | NHS Lanarkshire | £149.00 | 3 | £447.00 |
| Consultant appointment | Greater Glasgow & Clyde | £204.00 | 4 | £816.00 |
| Consultant appointment | NHS Lothian | £157.00 | 2 | £314.00 |
| GP appointment | Greater Glasgow & Clyde | £100.00 | 5 | £500.00 |
| A&E attendance | Greater Glasgow & Clyde | £135.00 | 2 | £270.00 |
| Haematology | Greater Glasgow & Clyde | £5.27 | 7 | £36.89 |
| Clinical chemistry | Greater Glasgow & Clyde | £0.91 | 10 | £9.10 |
| Urinalysis | Greater Glasgow & Clyde | £16.32 | 1 | £16.32 |
| Haematology | NHS Lanarkshire | £5.37 | 6 | £32.22 |
| Clinical chemistry | NHS Lanarkshire | £0.80 | 10 | £8.00 |
| Urinalysis | NHS Lanarkshire | £10.46 | 3 | £31.38 |
| Pathology | NHS Lanarkshire | £27.77 | 3 | £83.31 |
| Cancer markers | NHS Lanarkshire | £40.88 | 2 | £81.76 |
| Total | £11 482.74 |
*All costs from: http://www.isdscotland.org/Health-Topics/Finance/Costs/ (April 2016–March 2017).
Key: MRI, magnetic resonance imaging; CT, computerized tomography; GP, general practitioner; A&E, accident and emergency.
Itemized and total costs of investigative procedures for a patient with ACNES
| Procedure . | Health board . | Cost per item (£)* . | No. of items . | Total cost (£) . |
|---|---|---|---|---|
| Hysteroscopy (day surgery) | NHS Lanarkshire | £923.00 | 1 | £923.00 |
| Endoscopy (day surgery) | NHS Lanarkshire | £923.00 | 1 | £923.00 |
| Endoscopy (in-patient) 6 nights | Greater Glasgow & Clyde | £2625.00 | 1 | £2625.00 |
| Open exploration (in-patient) I night | NHS Lothian | £3511.00 | 1 | £3511.00 |
| MRI | NHS Lanarkshire | £188.92 | 1 | £188.92 |
| CT scan | NHS Lanarkshire | £83.74 | 1 | £83.74 |
| Abdominal ultrasound | NHS Lanarkshire | £43.08 | 1 | £43.08 |
| Vaginal ultrasound | Greater Glasgow & Clyde | £55.35 | 1 | £55.35 |
| Abdominal ultrasound | Greater Glasgow & Clyde | £55.35 | 1 | £55.35 |
| MRI | Greater Glasgow & Clyde | £214.16 | 2 | £428.32 |
| Consultant appointment | NHS Lanarkshire | £149.00 | 3 | £447.00 |
| Consultant appointment | Greater Glasgow & Clyde | £204.00 | 4 | £816.00 |
| Consultant appointment | NHS Lothian | £157.00 | 2 | £314.00 |
| GP appointment | Greater Glasgow & Clyde | £100.00 | 5 | £500.00 |
| A&E attendance | Greater Glasgow & Clyde | £135.00 | 2 | £270.00 |
| Haematology | Greater Glasgow & Clyde | £5.27 | 7 | £36.89 |
| Clinical chemistry | Greater Glasgow & Clyde | £0.91 | 10 | £9.10 |
| Urinalysis | Greater Glasgow & Clyde | £16.32 | 1 | £16.32 |
| Haematology | NHS Lanarkshire | £5.37 | 6 | £32.22 |
| Clinical chemistry | NHS Lanarkshire | £0.80 | 10 | £8.00 |
| Urinalysis | NHS Lanarkshire | £10.46 | 3 | £31.38 |
| Pathology | NHS Lanarkshire | £27.77 | 3 | £83.31 |
| Cancer markers | NHS Lanarkshire | £40.88 | 2 | £81.76 |
| Total | £11 482.74 |
| Procedure . | Health board . | Cost per item (£)* . | No. of items . | Total cost (£) . |
|---|---|---|---|---|
| Hysteroscopy (day surgery) | NHS Lanarkshire | £923.00 | 1 | £923.00 |
| Endoscopy (day surgery) | NHS Lanarkshire | £923.00 | 1 | £923.00 |
| Endoscopy (in-patient) 6 nights | Greater Glasgow & Clyde | £2625.00 | 1 | £2625.00 |
| Open exploration (in-patient) I night | NHS Lothian | £3511.00 | 1 | £3511.00 |
| MRI | NHS Lanarkshire | £188.92 | 1 | £188.92 |
| CT scan | NHS Lanarkshire | £83.74 | 1 | £83.74 |
| Abdominal ultrasound | NHS Lanarkshire | £43.08 | 1 | £43.08 |
| Vaginal ultrasound | Greater Glasgow & Clyde | £55.35 | 1 | £55.35 |
| Abdominal ultrasound | Greater Glasgow & Clyde | £55.35 | 1 | £55.35 |
| MRI | Greater Glasgow & Clyde | £214.16 | 2 | £428.32 |
| Consultant appointment | NHS Lanarkshire | £149.00 | 3 | £447.00 |
| Consultant appointment | Greater Glasgow & Clyde | £204.00 | 4 | £816.00 |
| Consultant appointment | NHS Lothian | £157.00 | 2 | £314.00 |
| GP appointment | Greater Glasgow & Clyde | £100.00 | 5 | £500.00 |
| A&E attendance | Greater Glasgow & Clyde | £135.00 | 2 | £270.00 |
| Haematology | Greater Glasgow & Clyde | £5.27 | 7 | £36.89 |
| Clinical chemistry | Greater Glasgow & Clyde | £0.91 | 10 | £9.10 |
| Urinalysis | Greater Glasgow & Clyde | £16.32 | 1 | £16.32 |
| Haematology | NHS Lanarkshire | £5.37 | 6 | £32.22 |
| Clinical chemistry | NHS Lanarkshire | £0.80 | 10 | £8.00 |
| Urinalysis | NHS Lanarkshire | £10.46 | 3 | £31.38 |
| Pathology | NHS Lanarkshire | £27.77 | 3 | £83.31 |
| Cancer markers | NHS Lanarkshire | £40.88 | 2 | £81.76 |
| Total | £11 482.74 |
*All costs from: http://www.isdscotland.org/Health-Topics/Finance/Costs/ (April 2016–March 2017).
Key: MRI, magnetic resonance imaging; CT, computerized tomography; GP, general practitioner; A&E, accident and emergency.
DISCUSSION
ACNES is clearly an underdiagnosed cause of abdominal wall pain [1, 8]. The reason why no one made the diagnosis was because no one thought of it [2]. Most patients with an eventual diagnosis of ACNES wait 6 years for the diagnosis; having had multiple scans and non-therapeutic operations [1, 7]. Previous estimates on unnecessary workup per patient with ACNES is over $6000, which is much less than c.£11 500 in this report [9].
The patient is a fit, healthy female, without relevant co-morbidities. She played two wind instruments, both held diagonally across the trunk and potentially shielding the right side of the abdomen from breathing pressures. This might have been the causal factor since overuse of the rectus muscle could be a mechanism for nerve entrapment [7]. Other causes include previous surgery with scarring, and ascites, obesity or pregnancy leading to increased intra-abdominal pressure and external compression [2, 7]. An important clinical feature was a positive Carnett’s sign as well as persistent point tenderness [5, 6].
This not-so-rare disorder is presented in order to spare future patients a protracted series of costly investigations. Diagnostic delays lead to excessive tests, invasive procedures and imaging studies, which cause psychological, physical and economic issues for patients [6]. The most damaging concern for this patient was whether her pain was actually believed by consulting physicians [4]. Playing wind instruments, especially those that demand a high level of forced expiration, should be added to the list of possible causes of ACNES. At a time when the NHS is keen to economize, healthcare authorities should consider the potential savings to be made by excluding ACNES for patients presenting with abdominal pain [10].
Acknowledgements
The patient approved full disclosure of clinical history, management, photograph and scans.
Funding
No funding was required for the writing of this article.
Conflicts of interest
No relevant conflict of interests reported by any author.
REFERENCES
- cost effectiveness
- exercise
- diagnostic services
- hernias
- laboratory techniques and procedures
- nerve compression syndrome
- neurons
- outpatients
- pain
- scotland
- surgical procedures, operative
- time factors
- diagnosis
- abdominal wall, anterior
- cost-effectiveness analysis
- abdominal cutaneous nerve entrapment syndrome
- national health service (uk)



