-
PDF
- Split View
-
Views
-
Cite
Cite
Ryan S Patton, Robert P Runner, David Lazarus, Thomas L Bradbury, Femoral neuropathy following direct anterior total hip arthroplasty: an anatomic review and case series, Journal of Surgical Case Reports, Volume 2018, Issue 9, September 2018, rjy171, https://doi.org/10.1093/jscr/rjy171
Close - Share Icon Share
Abstract
The popularity of the direct anterior approach for total hip arthroplasty (THA) has dramatically increased in recent years. Many patients request this muscle sparing approach for the theorized benefits of quicker recovery and reduced post-operative pain. Femoral nerve injury is a rare, yet serious complication following the anterior approach for THA. During the 7-year period from 2008 to 2016, 1756 patients underwent primary THA with a direct anterior approach by a single senior surgeon for end-stage osteoarthritis. Six (0.34%) of these patients had a post-operative femoral nerve palsy. We aim to discuss anatomic considerations, risk factors, and a timeline of severity and recovery for femoral nerve palsy following direct anterior THA in six patients.
INTRODUCTION
The femoral nerve (L2–L4) is the largest branch of the lumbar plexus. In the abdomen, the nerve originates within the psoas major and descends posterolaterally through the pelvis and deep to the midpoint of the inguinal ligament. After entering the femoral triangle laterally, the femoral nerve divides into several terminal motor branches to the anterior thigh muscles: pectineus, sartorius, illiacus and quadraceps femoris. It also sends sensory articular branches to the hip and knee joints and provides cutaneous innervation to the anteromedial thigh, terminating as the saphenous nerve. The saphenous nerve runs anteroinferiorly to supply the skin and fascia on the anteromedial aspects of the knee, leg and foot [1].
During the direct anterior approach (DAA) for total hip arthroplasty (THA), the tensor fascia is incised, and a deep dissection is made through the inter-nervous interval between the rectus femoris (femoral n.) and the gluteus medius (superior gluteal n.) [2, 3]. The rectus femoris is retracted medially often via an anterior acetabular retractor placed deep to the iliocapsularis over the anterior pelvic brim just medial to the iliopectineal eminence. After the anterior capsulotomy or capsulectomy and femoral neck osteotomy, this retractor is replaced deep to the capsule hugging the anterior wall of the acetabulum and riding over the anterior pelvic brim to expose the acetabulum for reaming and the gluteus medius is retracted laterally [2, 3]. Misplacement of the retractor either superficial to the iliopsoas or through its muscle bulk at the pelvic brim could result in the retractor tip lying over the femoral nerve [3].
Femoral nerve palsy can be a difficult problem for patients with symptoms including hypoesthesia, painful paresthesias or paralysis. These symptoms can have a profound effect on patient quality of life independent of the function of their THA, and the patient may never have full resolution [4]. While multiple explanations have been suggested, the etiology of femoral nerve palsy using the anterior approach remains difficult to ascertain [1]. We aim to discuss anatomic considerations, risk factors for nerve palsy and a timeline of severity and recovery for femoral nerve palsy following direct anterior THA in six patients.
CASE REPORT
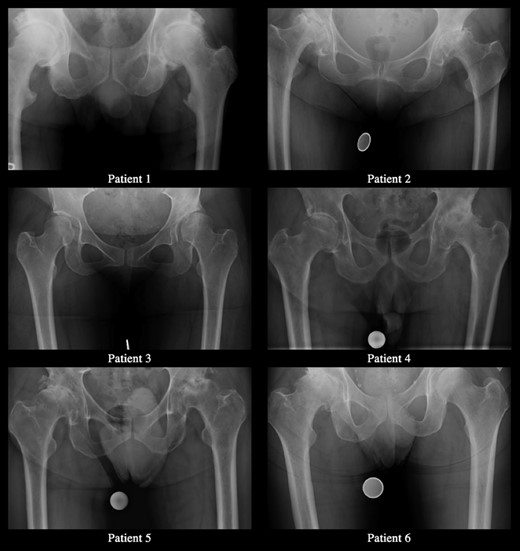
All patients underwent a DAA THA complicated by immediate post-operative femoral nerve palsy. Clinical characteristics are summarized in Table 1. Preoperative radiographs are exhibited in Fig. 1.
| Patient . | Clinical characteristics . | Final HOOS-JR . | Final DN4 . |
|---|---|---|---|
| 1 | 63-yo male. Left | 76.776 | 0 |
| Sensory: 6-wk: Distal anterior thigh deficit. 11-mo: Persistent diminished sensation over the anteromedial thigh. | |||
| Motor: 6-wk: Stiff-legged gait with walker. No active quadriceps function. 3-mo: Ambulating with cane. Re-innervation activity in the quadriceps by EMG. Active leg extension with less than anti-gravity strength. 6-mo: Stopped using cane. 4+/5 quadriceps strength. 11-mo: Normal gait with active and full leg extension. | |||
| 2 | 81-yo female. Right | 85.257 | 1 |
| Sensory: 3-mo: No deficit. | |||
| Motor: 6-wk: Presented in wheelchair with no active quadriceps function. Weak and difficult to assess abductors. 3-mo: Good hip flexor and abductor strength. No active knee extension. 6-mo: Active knee extension with 30° lag. 9-mo: Excellent rotational ROM with 4+/5 quadriceps strength and minimal comparative VMO atrophy. | |||
| 3 | 41-yo female. Left | ||
| Sensory: 6-wk: Sensitive to touch over thigh and knee with reduced sensation over distal anterior thigh and medial knee. 13-mo: Persistent diminished sensation. | |||
| Motor: 6-wk: No active quadriceps function. Diminished patellar DTR. 3-mo: Axonal femoral neuropathy with lack of femoral response on EMG. 7-mo: Good hip flexor and abductor strength with 3/5 quadriceps strength. 8-mo: 4+/5 quadriceps strength. 13-mo: 5−/5 quadriceps strength and minimal comparative VMO atrophy. | |||
| 4 | 78-yo male. Left | 100 | 1 |
| Sensory: 9-mo: Numbness from mid-thigh to knee. | |||
| Motor: 6-wk: Unable to actively extend knee. 9-mo: 5−/5 quadriceps strength. Able to perform single left leg squat. | |||
| 5 | 51-yo male. Left | 64.664 | 5 |
| Sensory: 1-wk: Perceived tingling over distal thigh with intact sensation. 6-wk: Small residual deficit over patella. | |||
| Motor:1-wk: No active quadriceps function. Fitted with transcutaneous electrical nerve stimulators (TENS) unit. 3-wk: 4−/5 quadriceps strength. 6-wk: Good hip flexor and abductor strength with 5/5 quadriceps strength. Performed single left leg squat. | |||
| 6 | 62-yo male. Right | 85.257 | 0 |
| Sensory: 2-wk: Distal anterior thigh deficit. 12-mo: No deficit. | |||
| Motor: 2-wk: Good hip flexor and abductor strength with 2/5 quadriceps strength. 3-wk: Initiated swing towards knee extension. Unable to maintain anti-gravitational positioning. 6-wk: Lost to follow-up with reports that he was utilizing outpatient therapy and TENS unit. 12-mo: 5−/5 quadriceps strength. | |||
| Patient . | Clinical characteristics . | Final HOOS-JR . | Final DN4 . |
|---|---|---|---|
| 1 | 63-yo male. Left | 76.776 | 0 |
| Sensory: 6-wk: Distal anterior thigh deficit. 11-mo: Persistent diminished sensation over the anteromedial thigh. | |||
| Motor: 6-wk: Stiff-legged gait with walker. No active quadriceps function. 3-mo: Ambulating with cane. Re-innervation activity in the quadriceps by EMG. Active leg extension with less than anti-gravity strength. 6-mo: Stopped using cane. 4+/5 quadriceps strength. 11-mo: Normal gait with active and full leg extension. | |||
| 2 | 81-yo female. Right | 85.257 | 1 |
| Sensory: 3-mo: No deficit. | |||
| Motor: 6-wk: Presented in wheelchair with no active quadriceps function. Weak and difficult to assess abductors. 3-mo: Good hip flexor and abductor strength. No active knee extension. 6-mo: Active knee extension with 30° lag. 9-mo: Excellent rotational ROM with 4+/5 quadriceps strength and minimal comparative VMO atrophy. | |||
| 3 | 41-yo female. Left | ||
| Sensory: 6-wk: Sensitive to touch over thigh and knee with reduced sensation over distal anterior thigh and medial knee. 13-mo: Persistent diminished sensation. | |||
| Motor: 6-wk: No active quadriceps function. Diminished patellar DTR. 3-mo: Axonal femoral neuropathy with lack of femoral response on EMG. 7-mo: Good hip flexor and abductor strength with 3/5 quadriceps strength. 8-mo: 4+/5 quadriceps strength. 13-mo: 5−/5 quadriceps strength and minimal comparative VMO atrophy. | |||
| 4 | 78-yo male. Left | 100 | 1 |
| Sensory: 9-mo: Numbness from mid-thigh to knee. | |||
| Motor: 6-wk: Unable to actively extend knee. 9-mo: 5−/5 quadriceps strength. Able to perform single left leg squat. | |||
| 5 | 51-yo male. Left | 64.664 | 5 |
| Sensory: 1-wk: Perceived tingling over distal thigh with intact sensation. 6-wk: Small residual deficit over patella. | |||
| Motor:1-wk: No active quadriceps function. Fitted with transcutaneous electrical nerve stimulators (TENS) unit. 3-wk: 4−/5 quadriceps strength. 6-wk: Good hip flexor and abductor strength with 5/5 quadriceps strength. Performed single left leg squat. | |||
| 6 | 62-yo male. Right | 85.257 | 0 |
| Sensory: 2-wk: Distal anterior thigh deficit. 12-mo: No deficit. | |||
| Motor: 2-wk: Good hip flexor and abductor strength with 2/5 quadriceps strength. 3-wk: Initiated swing towards knee extension. Unable to maintain anti-gravitational positioning. 6-wk: Lost to follow-up with reports that he was utilizing outpatient therapy and TENS unit. 12-mo: 5−/5 quadriceps strength. | |||
| Patient . | Clinical characteristics . | Final HOOS-JR . | Final DN4 . |
|---|---|---|---|
| 1 | 63-yo male. Left | 76.776 | 0 |
| Sensory: 6-wk: Distal anterior thigh deficit. 11-mo: Persistent diminished sensation over the anteromedial thigh. | |||
| Motor: 6-wk: Stiff-legged gait with walker. No active quadriceps function. 3-mo: Ambulating with cane. Re-innervation activity in the quadriceps by EMG. Active leg extension with less than anti-gravity strength. 6-mo: Stopped using cane. 4+/5 quadriceps strength. 11-mo: Normal gait with active and full leg extension. | |||
| 2 | 81-yo female. Right | 85.257 | 1 |
| Sensory: 3-mo: No deficit. | |||
| Motor: 6-wk: Presented in wheelchair with no active quadriceps function. Weak and difficult to assess abductors. 3-mo: Good hip flexor and abductor strength. No active knee extension. 6-mo: Active knee extension with 30° lag. 9-mo: Excellent rotational ROM with 4+/5 quadriceps strength and minimal comparative VMO atrophy. | |||
| 3 | 41-yo female. Left | ||
| Sensory: 6-wk: Sensitive to touch over thigh and knee with reduced sensation over distal anterior thigh and medial knee. 13-mo: Persistent diminished sensation. | |||
| Motor: 6-wk: No active quadriceps function. Diminished patellar DTR. 3-mo: Axonal femoral neuropathy with lack of femoral response on EMG. 7-mo: Good hip flexor and abductor strength with 3/5 quadriceps strength. 8-mo: 4+/5 quadriceps strength. 13-mo: 5−/5 quadriceps strength and minimal comparative VMO atrophy. | |||
| 4 | 78-yo male. Left | 100 | 1 |
| Sensory: 9-mo: Numbness from mid-thigh to knee. | |||
| Motor: 6-wk: Unable to actively extend knee. 9-mo: 5−/5 quadriceps strength. Able to perform single left leg squat. | |||
| 5 | 51-yo male. Left | 64.664 | 5 |
| Sensory: 1-wk: Perceived tingling over distal thigh with intact sensation. 6-wk: Small residual deficit over patella. | |||
| Motor:1-wk: No active quadriceps function. Fitted with transcutaneous electrical nerve stimulators (TENS) unit. 3-wk: 4−/5 quadriceps strength. 6-wk: Good hip flexor and abductor strength with 5/5 quadriceps strength. Performed single left leg squat. | |||
| 6 | 62-yo male. Right | 85.257 | 0 |
| Sensory: 2-wk: Distal anterior thigh deficit. 12-mo: No deficit. | |||
| Motor: 2-wk: Good hip flexor and abductor strength with 2/5 quadriceps strength. 3-wk: Initiated swing towards knee extension. Unable to maintain anti-gravitational positioning. 6-wk: Lost to follow-up with reports that he was utilizing outpatient therapy and TENS unit. 12-mo: 5−/5 quadriceps strength. | |||
| Patient . | Clinical characteristics . | Final HOOS-JR . | Final DN4 . |
|---|---|---|---|
| 1 | 63-yo male. Left | 76.776 | 0 |
| Sensory: 6-wk: Distal anterior thigh deficit. 11-mo: Persistent diminished sensation over the anteromedial thigh. | |||
| Motor: 6-wk: Stiff-legged gait with walker. No active quadriceps function. 3-mo: Ambulating with cane. Re-innervation activity in the quadriceps by EMG. Active leg extension with less than anti-gravity strength. 6-mo: Stopped using cane. 4+/5 quadriceps strength. 11-mo: Normal gait with active and full leg extension. | |||
| 2 | 81-yo female. Right | 85.257 | 1 |
| Sensory: 3-mo: No deficit. | |||
| Motor: 6-wk: Presented in wheelchair with no active quadriceps function. Weak and difficult to assess abductors. 3-mo: Good hip flexor and abductor strength. No active knee extension. 6-mo: Active knee extension with 30° lag. 9-mo: Excellent rotational ROM with 4+/5 quadriceps strength and minimal comparative VMO atrophy. | |||
| 3 | 41-yo female. Left | ||
| Sensory: 6-wk: Sensitive to touch over thigh and knee with reduced sensation over distal anterior thigh and medial knee. 13-mo: Persistent diminished sensation. | |||
| Motor: 6-wk: No active quadriceps function. Diminished patellar DTR. 3-mo: Axonal femoral neuropathy with lack of femoral response on EMG. 7-mo: Good hip flexor and abductor strength with 3/5 quadriceps strength. 8-mo: 4+/5 quadriceps strength. 13-mo: 5−/5 quadriceps strength and minimal comparative VMO atrophy. | |||
| 4 | 78-yo male. Left | 100 | 1 |
| Sensory: 9-mo: Numbness from mid-thigh to knee. | |||
| Motor: 6-wk: Unable to actively extend knee. 9-mo: 5−/5 quadriceps strength. Able to perform single left leg squat. | |||
| 5 | 51-yo male. Left | 64.664 | 5 |
| Sensory: 1-wk: Perceived tingling over distal thigh with intact sensation. 6-wk: Small residual deficit over patella. | |||
| Motor:1-wk: No active quadriceps function. Fitted with transcutaneous electrical nerve stimulators (TENS) unit. 3-wk: 4−/5 quadriceps strength. 6-wk: Good hip flexor and abductor strength with 5/5 quadriceps strength. Performed single left leg squat. | |||
| 6 | 62-yo male. Right | 85.257 | 0 |
| Sensory: 2-wk: Distal anterior thigh deficit. 12-mo: No deficit. | |||
| Motor: 2-wk: Good hip flexor and abductor strength with 2/5 quadriceps strength. 3-wk: Initiated swing towards knee extension. Unable to maintain anti-gravitational positioning. 6-wk: Lost to follow-up with reports that he was utilizing outpatient therapy and TENS unit. 12-mo: 5−/5 quadriceps strength. | |||
DISCUSSION
Merits of direct anterior approach, also known as anterior iliofemoral or Smith-Peterson, or the modification to the Hueter approach for THA include dissection through inter-nervous planes and avoidance of disruption of abductor mechanisms [2]. However, as in all surgical approaches, it has opportunity for adverse outcomes.
In the literature, the prevalence of motor nerve palsy after anterior THA has been reported to range from 0.3 to 3.7%, and from 0.1 to 0.4% for the femoral nerve specifically [4, 5]. During a 7-year period from 2008 to 2016, 1756 consecutive patients underwent primary THA via a direct anterior Hueter approach in a single center by a single surgeon to correct end-stage osteoarthritis. Six (0.34%) of these patients were found to have a post-operative femoral nerve palsy. Despite a relatively low incidence, femoral neuropathy following primary THA presents significant morbidity. In a 2005 study of 27 004 primary THA, Farrell [4] reported 47 cases of motor nerve palsy with only 17 patients (36%) attaining complete recovery of motor strength, which took an average of 21.1 months. Of our six patients, all recovered motor strength with timeline to recovery ranging from 6 weeks to 13 months as demonstrated in Table 1.
The proposed etiology for neuropathy after THA includes direct trauma, excessive tension during extremity lengthening, direct contact with methylmethacrylate or the heat of its polymerization, constriction by wire fixation, femoral component dislocation, ischemia, and compression; however, in most patients the actual cause has not been determined [1, 4, 6]. Weale et al. [7] hypothesized that anterior retractors placed around the acetabulum were responsible for subclinical damage to the femoral nerve. As the femoral nerve passes distal to the inguinal ligament, it is in close proximity to the anterior wall of the acetabulum, traveling on average 1.8–2.2 cm from the anterior lip [3, 8]. With only the iliopsoas between the anterior capsule and the femoral nerve, any retractor misplacement or repositioning places the nerve at risk of compression directly or by proxy if the retractor is placed through the iliopsoas bulk. All six of our patients had multiple, large, anterior osteophytes as evidenced by preoperative radiographs in Fig. 1, which we believe may have contributed to difficulty attaining or maintaining direct contact between the anterior retractor and the wall of the anterior acetabulum, putting the femoral nerve at risk.
We encourage exercising caution in the placement of acetabular retractors during anterior THA to avoid femoral nerve compression. Furthermore, we suggest careful consideration of osteophytosis and its implications in acetabular retractor placement during preoperative planning. Lastly, identification of femoral neuropathy in the early post-operative period is important for communication of recovery expectations and therapeutic planning with patients.
Conflict of Interest statement
Each author certifies that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangements) that might pose a conflict of interest in connection with the submitted article.
REFERENCES
Author notes
Investigation performed at Emory University Department of Orthopaedics.



