-
PDF
- Split View
-
Views
-
Cite
Cite
Erion Qaja, Michael Segal, Christopher Engler, Mohan Badhey, Mahalingam Sivakumar, Retrograde embolization of anterior tibial artery for an iatrogenic arterio-venous fistula causing left lower extremity claudication, Journal of Surgical Case Reports, Volume 2018, Issue 8, August 2018, rjy219, https://doi.org/10.1093/jscr/rjy219
Close - Share Icon Share
Abstract
Lower extremity angiogram is generally a safe and effective procedure with a low rate of vascular complications. We report here a unique case of a 33-year-old female with anterior tibial artery (ATA) to anterior tibial vein fistula formation after lower extremity endovascular intervention. This was initially treated with open repair of the fistula and ligation of ATA. However, patient continued to complain of claudication like symptoms. Patient subsequently had an endovascular embolization of ATA in a retrograde fashion. Recovery was unremarkable; patient was discharged home same day. Three months postoperatively patient denies leg pain, a follow-up arterial duplex failed to show presence of arterio-venous fistula. This case illustrates the effectiveness of an endovascular approach as a minimally invasive treatment for this uncommon complication that occurs after lower extremity endovascular intervention.
INTRODUCTION
Iatrogenic arterio-venous fistula (AVF) creations of lower extremity are uncommon complications of endovascular interventions of lower extremity. They are often recognized either on repeat arteriograms of lower extremity or CT angiogram as patients usually complain of lower extremity claudication, non-healing ulcers or ongoing tissue loss. The pathophysiology of claudication is based on the steal phenomenon, which is the hallmark of AVF. Aortogram would delineate the arterial tree with delayed retrograde filling of deep venous system. A bruit is rarely clinically evident especially deep in the calf muscle. Once identified, AVF should be promptly surgically treated [1]. We present a case of a 33-year-old female that was successfully treated with retrograde embolization of ATA for an iatrogenic AVF caused by previous endovascular interventions in left lower extremity. Patient was discharged home same day and her recovery has been unremarkable with complete resolution of her right lower extremity claudication.
CASE REPORT
Patient is a 33-year-old female with a past medical history of systemic lupus erythematosus (SLE) and lower extremity deep venous thrombosis (DVT). She has been treated with oral anticoagulants for her lower extremity DVT with complete resolution of thrombus in 6 months venous duplex ultrasound follow up. Her past surgical history is significant for a left lower extremity angiogram with a stent placed in distal superficial femoral artery (SFA). It is unclear what prompted her lower extremity intervention, as patient had no stigmata of peripheral arterial disease clinically or in arterial duplex studies. Her only complain at that time was calf pain; most likely related to her DVT in left popliteal vein. She was seen in clinic with left calf pain, mild swelling of left lower extremity and three blocks claudication of the ipsilateral leg. Her clinical exam did not show evidence of tissue loss, there was swelling of left calf, a dopplerable dorsalis pedis (DP) pulse and a palpable posterior tibial (PT) pulse with sluggish capillary refill and a warm left foot. Patient subsequently underwent arterial duplex studies which showed ABI of 1.13 on the left, presence of high output ATA to anterior tibial vein (ATV) fistula, biphasic flow in the left femoral vein, patent SFA, popliteal artery (PA), with three vessel run off to the foot. In comparison right lower extremity had unremarkable arterial duplex studies as one should suspect in a young, non-smoker female.
Patient underwent an open ligation of AVF ~6 months since her diagnosis. ATA was ligated proximally at the take off by a medial surgical approach. Routine postoperative surveillance was significant for persistent claudication and left calf swelling. A repeat arterial duplex study revealed yet again the presence of AVF.
Surgical options were discussed with patients including another open repair vs. retrograde embolization. We decided that embolization would delineate the AVF site much clearer and efficient embolization of the entire fistulous tract could be achieved as live images are visualized under fluoroscopy. Minimal invasive nature of the procedure made the latter option much more appealing to the patient.
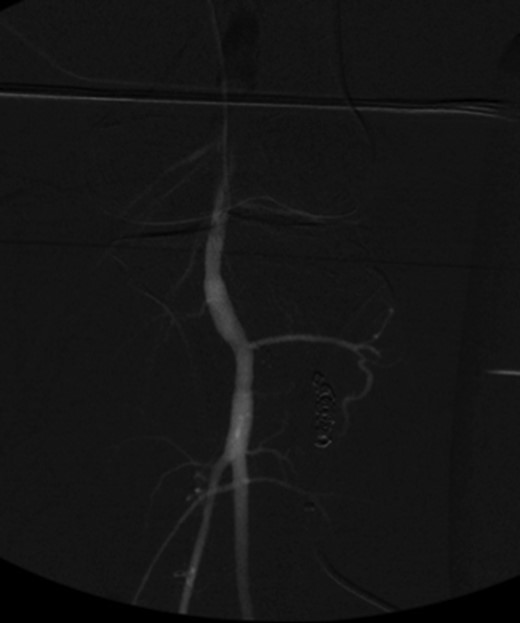
Patient underwent a left lower extremity angiogram. During the procedure she was found to have patent aorta and bilateral common iliac artery. There was no disease visualized in the left external iliac artery, common femoral artery (CFA), SFA, patent previously placed stent, patent above and below the knee PA and two vessel run off to the foot (Fig. 1). Upon delayed fluoroscopic images we identified contrast filling the deep venous system rather quickly suggesting a high volume fistula (Fig. 2). We then identified the fistula between ATA and ATV. Although ATA was previously ligated there was retrograde filling of the artery from unnamed branches, which communicated with the venous system as shown in. In the midcalf (ATA) was cannulated with a micropuncture needle. Micropuncture wire was inserted and a 5-Fr sheath was inserted after exchanging over wire. At this point VortX coils (Boston Scientific) were placed from the curve of ATA until the whole AVF was sealed. Anterograde angiogram showed no flow through the fistula (Figs 3 and 4). There was a palpable PT and DP pulse at the completion of the procedure. Sheath was removed, pressure dressing applied. Patient was discharged home same day. Recovery has been unremarkable. Three months follow-up claudication symptoms have significantly improved.
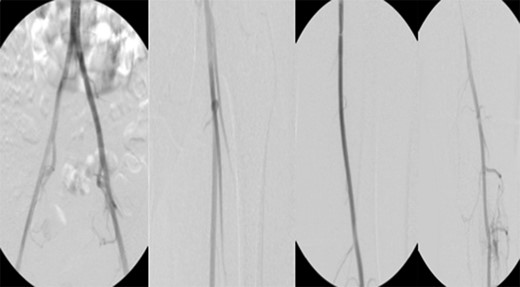
Fluoroscopy showing; left external iliac artery (EIA), common femoral artery (CFA), superficial femoral artery (SFA), patent previously placed stent, patent above and below the knee popliteal artery (PA) and two vessel run off to the foot.

Fluoroscopy imaging showing high volume anterior tibial artery to vein iatrogenic fistula.

VortX coils (Boston Scientific) were placed from the curve of anterior tibial artery to its communication with venous system.
Anterograde angiogram showed no flow through the fistula tract with two vessels run off.
DISCUSSION
Iatrogenic AVF of the infrapopliteal vessels are uncommon on patients undergoing endovascular interventions of the lower extremity. There are site entry complications such as pseudoaneruysm, CFA dissections, retroperitoneal bleeding and embolizations [2]. However, to our knowledge infrapopliteal AVF has not been described in literature. We have presented a case of ATA to ATV fistula formation. It is our suspicion that this AVF was caused due to patient’s prior endovascular interventions with SFA stent placement. Perhaps an injury to the artery and vein during wire passage on initial angiogram could have been the culprit, albeit a speculative assessment. The amount of high flow noted on repeat arterial duplex as well as angiogram caused a considerable amount of steal phenomena on patient left foot resulting in life style limiting claudication. When AVF cause symptoms then they would need repair whether be it open or endovascular approach. Our patient did go repair initially with ligation and clipping of ATA. She initially showed some improvement. Over the course of time ATA was being filled through collaterals with subsequent expansion of fistulous tract and increase in flow of the fistula. During the second intervention patient underwent retrograde endovascular embolization of ATA with satisfactory results.
There are no clear data on how to manage iatrogenic AVF creation. Whereas it is acceptable clinical practice to closely observe asymptomatic AVF with serial arterial duplex and physical examination. Any symptomatic AVF should undergo repair [3, 4]. Whether it is done open vs endovascular will depend on overall medical condition of the patient. Typically endovascular approach is reserved for the high-risk surgical patient and/or those who have failed open surgical intervention [5]. There are drawbacks, however, to endovascular approach. One potential complication is coil migration to the venous system resulting with deep venous system thrombosis and devastating sequela of leg edema. Moreover, migration of coils could happen in arterial system as well with potential occlusion of the proximal arterial tree. We were able to perform a coil embolization rather safely given the risk of proximal coil migration was non existent since ATA was already clipped during open ligation of the fistula. There is no clear consensus as to which approach should be attempted first [6]. In summary, it is our preference patient undergoes open fistula ligation due to high complication rate of endovascular embolization and unexpected coil migration.
AUTHOR’S CONTRIBUTIONS
All coauthors have seen and agree with the contents of the article. We certify that the submission is original work and has not been published previously elsewhere.
CONFLICTS OF INTEREST STATEMENT
None declared.



