-
PDF
- Split View
-
Views
-
Cite
Cite
David P Mysona, Thomas L Estes, Age is nothing but a number: radical en bloc resection of colon adenocarcinoma with abdominal wall reconstruction in an 81 year old, Journal of Surgical Case Reports, Volume 2018, Issue 8, August 2018, rjy206, https://doi.org/10.1093/jscr/rjy206
Close - Share Icon Share
Abstract
Colon adenocarcinoma is a common neoplasm, which rarely presents with full thickness invasion through the abdominal wall. Aggressive treatment is often reserved for younger patients, with many surgeons opting to consider elderly patients as non-operative candidates, especially in the setting of diffuse disease. We report a case of radical resection of a colon cancer, with full thickness abdominal wall invasion in an 81-year-old female. The patient presented with gradual abdominal swelling over multiple months. She had a CT scan revealing a mass eroding through her abdominal wall, up to the skin. Operative resection with adjuvant chemotherapy was chosen as therapy because the patient had no co-morbidities. The patient underwent en bloc resection of the abdominal wall with right hemicolectomy and resection of all structures attached to the mass. The patient has been disease free for 24 months and has had return to her baseline activities of daily living.
INTRODUCTION
Colon cancer is a major contributor to cancer mortality every year. In 2016, colon cancer was the third most common malignancy among men and women with ~130 000 new cases and was third in number of cancer mortalities, causing almost 50 000 deaths [1]. Over half of colon cancers are diagnosed in patients >70 years old. However, despite being more often diagnosed in the elderly, there is less knowledge regarding the disease and optimal treatment in this population of patients [2, 3].
Colon cancer treatment revolves around chemotherapy in combination with surgical resection. The main goal of surgery is to accomplish staging and aggressively remove all disease. Unfortunately, multiple studies have shown that elderly patients are often treated differently, with surgeons and oncologists commonly opting for less aggressive treatment options resulting in worse outcomes [3]. In fact, in a retrospective study by Lemmens et al. [4], even though 26% of 842 patients >80 years old had no co-morbidities, only 0.2% of the 842 received both surgery and chemotherapy. The decreased optimal management of elderly patients is troubling, given multiple studies have shown that age is not an independent risk factor for poor treatment outcomes [2–4]. The following case is a rare presentation of colorectal cancer and supports that age is merely a number when treating this disease.
CASE REPORT
An 81-year-old female presented to her primary care provider secondary to gradual abdominal swelling over multiple months. Her past medical history included gastroesophageal reflux disease and hypertension. The patient had no other significant history. Of note, the patient was living independently, fully active, and able to care for herself, giving her an ECOG performance status of 0. Her physical exam revealed a 12 cm palpable mass in the right lower quadrant (Fig. 1). At that time, the patient was sent for a computed tomography (CT) scan.

Initial physical exam of the patient revealed a palpable mass in the abdomen along with obvious skin erythema and irritation most likely secondary to the mass located just below the skin.
CT scan showed a mass arising from the right colon eroding through the abdominal wall almost to the level of skin (Fig. 2A and B). Of note, the scan showed no evidence of distant metastases. The patient was referred for surgical evaluation and desired definitive treatment. The patient was not a candidate for full length colonoscopy secondary to severe diverticular disease and segmental stenosis.
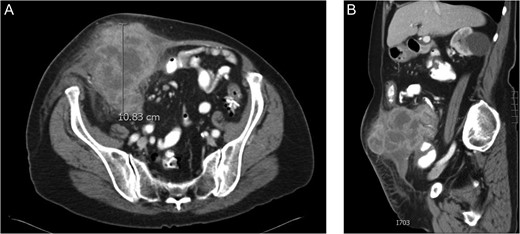
(A) CT scan of the abdomen in cross section revealing a large right sided colon cancer eroding through the rectus sheath almost to the level of the skin. As seen in the image, the patient was not obstructed at the time of presentation. (B) CT scan showing the mass from a sagittal perspective. The liver had no evidence of metastasis.
The patient underwent radical resection of the involved right abdominal wall (30 cm × 15 cm), resection of cecal mass (20 cm × 10 cm), and all attached anatomic structures to the mass including right oophorectomy, right hemicolectomy, and resection of 3 feet of ileum (Figs 3 and 4). The right abdominal wall was then reconstructed using biologic XenMatrix mesh (20 cm × 15 cm).
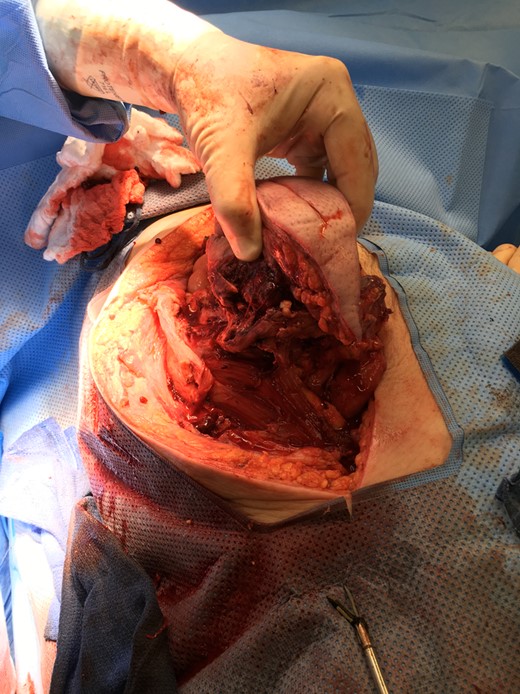
An initial elliptical incision was made measuring ~15 cm in length. The incised abdominal wall was then mobilized to provide exposure of intra-abdominal structures attached to the mass. All attached structures were removed en bloc with the abdominal wall mass.

En bloc specimen of the abdominal wall mass, three feet of ileum, and right hemicolectomy (right ovary not shown).
Pathology showed a colon adenocarcinoma and lymph node metastases within the mesentery. The patient was staged as 3 C (T4b N2 M0). Her abdominal wall on 6-week post-op visit had no defects or evidence of hernias (Fig. 5). At this time, she had returned to her baseline ECOG performance status without requiring home health or physical therapy. She went on to receive 11 cycles of FOLFOX (folinic acid, fluorouracil, oxiplatin) chemotherapy. On recent follow up, 24 months post-surgery, the patient was disease free. Her abdominal wall reconstruction has remained successful without hernias.

Abdomen on 6-week post-op follow up showed no evidence of hernia and had an appropriate healing midline incision.
DISCUSSION
Adenocarcinoma of the colon is a commonly encountered neoplasm. However, this case is uncommon because patient presented with stage 4Tb disease secondary to full thickness abdominal wall invasion. She then went on to have radical surgery and adjuvant chemotherapy. Furthermore, current literature shows that elderly patients with colonic neoplasms are often under treated for a variety of reasons. However, multiple studies have shown that age alone is not a prognostic factor, but multiple co-morbidities are a measure of prognosis [2–4]. Given this information, elderly patients with few co-morbidities and appropriate independent function should be offered standard treatment when diagnosed with colon cancer. This case required critical decision making using both advice from current literature regarding treatment of colorectal cancer and the repair of abdominal wall defects.
Patients with pT4a and pT4b colorectal tumors have shown to have varying prognosis based on the margin of cancer left behind during surgery [3, 5]. An R0 resection, complete tumor resection with all margins negative, is associated with improved survival risk of relapse and is currently the standard [3]. R0 resections have shown to have a dramatic impact on prognosis with 5-year disease free survival in the R0 group being as high as 76% versus 32% R1 resections, microscopic margin involvement [6]. This difference persists when examining overall survival with R0 patients having 60% 5-year overall survival versus 25% in R1 resections [6]. Furthermore, an R0 resection of pT4 tumors has been shown to result in equivalent outcomes as if the patient had a smaller tumor (pT3) [5]. This trend holds true when considering metastatic disease.
Multiple studies have demonstrated that resection of colon cancer metastases results in improved survival. Furthermore, the use of neoadjuvant chemotherapy to achieve an R0 resection has shown to result in an improved survival for patients [7]. Research has also shown elderly patients treated with surgical resection have better survival compared to those who do not undergo resection and only receive chemotherapy [8]. Furthermore, patients with an age >75 who undergo surgical resection have been shown to have equivalent benefits of adjuvant chemotherapy without increased toxicity when compared to younger patients [9]. Given this information, the preferred option would have been neoadjuvant therapy followed by surgery. This would have allowed for a safer surgery with equivalent outcomes. However, secondary to concern for abdominal infection, possible cellulitis, and concern that the mass would soon penetrate through the epidermis, the decision was made to proceed with surgery and abdominal wall reconstruction.
Biologic and synthetic mesh are products commonly used to aide in abdominal wall reconstruction. A major limitation to synthetic mesh is that it is not recommended to be placed in a contaminated field [10]. Since the patient had a large colonic mass eroding through the abdominal wall, contamination could not be ruled out. Thus a biologic mesh was chosen instead of a synthetic mesh because biologic meshes have been shown to be safe and feasible in a contaminated field. However, long term durability has not been proven when placed in a contaminated field [10]. Despite the patient being at an increased risk of a ventral hernia in the future, her 24-month disease free survival far outweighs the risk of a potential future hernia.
In conclusion, this case provides encouragement that elderly patients with few co-morbidities can successfully undergo radical cancer surgery and adjuvant chemotherapy, with complete return to baseline function. However, it is important to integrate multiple factors when determining when and when not to operate. These factors include potential of an R0 resection, the role of neoadjuvant chemotherapy if an R0 resection is not considered achievable at the time of presentation, as well as, patient co-morbidities and patient performance status. This case will hopefully serve to generate further conversation that age alone is not a candidate for decreased aggressiveness in treatment of cancer.
ACKNOWLEDGEMENTS
Thankful for the patient providing consent to present her case.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
No funding requirements.



