-
PDF
- Split View
-
Views
-
Cite
Cite
Vitor Augusto de Andrade, Cláudio Saddy Rodrigues Coy, João José Fagundes, Pedro França da Costa Soares, Maria de Lourdes Setsuko Ayrizono, Carlos Augusto Real Martinez, Paraestomal hernia with gastric outlet obstruction: a case report and literature review, Journal of Surgical Case Reports, Volume 2018, Issue 7, July 2018, rjy177, https://doi.org/10.1093/jscr/rjy177
Close - Share Icon Share
Abstract
An 69-year-old obese woman was submitted to an abdominoperineal resection (APR) with left side end colostomy to treat a synchronic sigmoid and middle rectum cancer. Six months after APR, she develop a PH with a progressive increase of the size. The patient refused the surgical indication. Thirteen years after APR she presenting with abdominal pain, hematemesis, bilious vomiting and non-functioning of the stoma in the last 2 days. She had a distended and painful abdomen without signs of peritoneal irritation and a large incarcerated PH. CT showed a PH with incarcerated gastric herniation. Endoscopy showed a 4 cm ulcerated lesion in the lesser curvature of the stomach whose posteriorly histopathological study revealed that it was an ischemic ulcer. She was submitted a correction of PH using an onlay polypropylene mesh put around of the previous stoma. The patient has an uneventful recovery and was discharged 3 days later.
INTRODUCTION
Parastomal hernia (PH) is one of the most common and significant complications following stoma formation. It has been showed that PH develops in up to 78% of patients with a stoma and typically occurs within 2 years of ostomy creation but may develop as long as 20 or 30 years after surgery. The presence of the stomach inside of PH causing a gastric outlet obstruction is an exceptional finding. To the best of our knowledge there are only nine cases described to date in worldwide literature [1–9]. The aim of this report is to describe a case of gastric outlet obstruction due to stomach incarceration inside of the PH successfully treated by an onlay repair with a polypropylene mesh placed by the site of the ostomy.
CASE REPORT
A 77-year-old woman was submitted 13 years before to end colostomy in left flank due to abdominoperineal resection (APR) resection to treat a synchronic sigmoid and middle rectal adenocarcinoma. She was admitted at the ER presenting a 2 days history of diffuse abdominal pain associated with hematemesis and non-functioning stoma. An irreducible and painfully PH was identified on left side of the abdomen (Fig. 1).

Incarcerated PH located in left side abdominal at the site of a terminal colostomy.
An abdominal computed tomography (CT) demonstrated a voluminous PH with part of the stomach protruded through the PH (Fig. 2A and B).
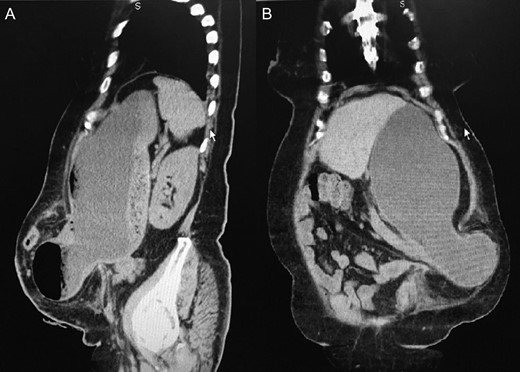
(A) Sagital view of the PH containing the distal part of the stomach. (B) Coronal view of the PH with gastric content in inferior left side of the abdomen.
With the diagnosis of gastric output obstruction, it was decided to perform a digestive upper endoscopy to clarify the cause of the digestive bleeding. The endoscopy identify a diffuse erosive gastritis and an ulcerated lesion with 4 cm of diameter. The patient was submitted to paraestomal herniorrhaphy performed through an arciform incision done in the lower and lateral side of the stoma similarly to that previously performed by other author [10]. After release of the adhesions the stomach was easily returned to the abdominal cavity. The fascial defect was closed with a single layer of interrupted polypropylene sutures (Ethicon™, Johnson & Johnson, USA). The PH was corrected using an onlay polypropylene mesh (Propy-Mesh, Atramat™, Mexico), cut like an ‘M’ letter (Fig. 3A). The lateral large flaps of the ‘M’ mesh were passed alongside the lateral walls of the colon and fixed at colonic wall with interrupted stiches of 3-0 polypropylene (Ethicon™, Johnson & Johnson, USA) and the central part of the ‘M’ letter mesh crossed the mesocolon between the mesenteric border of the colonic wall and the marginal arterial arcade. The three flaps of the ‘M’ mesh were fixed on the aponeurosis of the external oblique and rectus abdominis muscles with suture with uninterrupted suture of prolene 2-0 (Ethicon™, Johnson & Johnson, USA) (Fig. 3B). After PH repair, the patient presented a satisfactory evolution, being discharged on the third postoperative day, with follow-up without relapse of PH 12 months after the procedure.
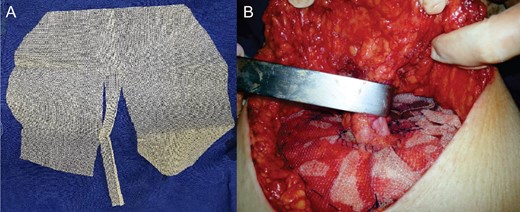
(A) Polypropylene mesh, cut like a letter ‘M’. (B) Final aspect of onlay mesh paraestomal hernioplasty.
DISCUSSION
It was estimate that 450 000 people currently lives with a stoma in USA and 120 000 new stomas were created each year and the number of patients submitted to an ostomy grow at annual rate of 3%. PH is the most frequent late complication following stoma creation and its prevalence is only expected to increase. A literature review found that PH occur in 4.0–48.1% of patients with end colostomies [10].
The mainly contents presents inside of the hernia sac include omentum, small bowel and colon. The presence of the stomach inside a PH is exceptionally rare with only a few published cases in international literature (Table 1) [1–9]. To the best of our knowledge, the patient presented in this publication represents only the 10th case described.
| Author/year . | Age (y) . | Sex . | Initial procedure . | Access way . | Technique of PH correction . | Mesh . | Outcomes . |
|---|---|---|---|---|---|---|---|
| Figiel and Figiel, 1967 | 76 | F | Loop colostomy | Laparotomy | Primary repair | No | Deceased |
| McAllister and D’Altorio, 1991 | 91 | F | End colostomy | Laparotomy | Stoma transposition | No | Discharge |
| Ellingson et al., 1993 | 77 | F | End colostomy | – | Primary repair | No | Discharge |
| Bota et al., 2012 | 41 | F | End ileostomy | Laparotomy | Primary repair | Yes | Mesh infection |
| Ilyas et al., 2012 | 93 | F | End colostomy | Laparotomy | Primary repair | No | Discharge |
| Ramia-Angel et al., 2012 | 64 | F | End colostomy | Refuse operative repair | None | No | Discharge |
| Marsh and Hoejgaard, 2013 | 81 | M | End colostomy | Laparotomy | Stoma transposition | No | Wound infection |
| Barber-Millet et al., 2014 | 69 | F | End colostomy | Laparotomy | Stoma transposition Preventive mesh of the new stoma | Yes | Discharge |
| Bull et al., 2017 | 85 | F | Loop colostomy | Laparoscopy convert to laparotomy | Stoma transposition | No | Discharge |
| Andrade et al., 2017 (current report) | 77 | F | End colostomy | Stoma site | Primary repair | Yes | Discharge |
| Author/year . | Age (y) . | Sex . | Initial procedure . | Access way . | Technique of PH correction . | Mesh . | Outcomes . |
|---|---|---|---|---|---|---|---|
| Figiel and Figiel, 1967 | 76 | F | Loop colostomy | Laparotomy | Primary repair | No | Deceased |
| McAllister and D’Altorio, 1991 | 91 | F | End colostomy | Laparotomy | Stoma transposition | No | Discharge |
| Ellingson et al., 1993 | 77 | F | End colostomy | – | Primary repair | No | Discharge |
| Bota et al., 2012 | 41 | F | End ileostomy | Laparotomy | Primary repair | Yes | Mesh infection |
| Ilyas et al., 2012 | 93 | F | End colostomy | Laparotomy | Primary repair | No | Discharge |
| Ramia-Angel et al., 2012 | 64 | F | End colostomy | Refuse operative repair | None | No | Discharge |
| Marsh and Hoejgaard, 2013 | 81 | M | End colostomy | Laparotomy | Stoma transposition | No | Wound infection |
| Barber-Millet et al., 2014 | 69 | F | End colostomy | Laparotomy | Stoma transposition Preventive mesh of the new stoma | Yes | Discharge |
| Bull et al., 2017 | 85 | F | Loop colostomy | Laparoscopy convert to laparotomy | Stoma transposition | No | Discharge |
| Andrade et al., 2017 (current report) | 77 | F | End colostomy | Stoma site | Primary repair | Yes | Discharge |
| Author/year . | Age (y) . | Sex . | Initial procedure . | Access way . | Technique of PH correction . | Mesh . | Outcomes . |
|---|---|---|---|---|---|---|---|
| Figiel and Figiel, 1967 | 76 | F | Loop colostomy | Laparotomy | Primary repair | No | Deceased |
| McAllister and D’Altorio, 1991 | 91 | F | End colostomy | Laparotomy | Stoma transposition | No | Discharge |
| Ellingson et al., 1993 | 77 | F | End colostomy | – | Primary repair | No | Discharge |
| Bota et al., 2012 | 41 | F | End ileostomy | Laparotomy | Primary repair | Yes | Mesh infection |
| Ilyas et al., 2012 | 93 | F | End colostomy | Laparotomy | Primary repair | No | Discharge |
| Ramia-Angel et al., 2012 | 64 | F | End colostomy | Refuse operative repair | None | No | Discharge |
| Marsh and Hoejgaard, 2013 | 81 | M | End colostomy | Laparotomy | Stoma transposition | No | Wound infection |
| Barber-Millet et al., 2014 | 69 | F | End colostomy | Laparotomy | Stoma transposition Preventive mesh of the new stoma | Yes | Discharge |
| Bull et al., 2017 | 85 | F | Loop colostomy | Laparoscopy convert to laparotomy | Stoma transposition | No | Discharge |
| Andrade et al., 2017 (current report) | 77 | F | End colostomy | Stoma site | Primary repair | Yes | Discharge |
| Author/year . | Age (y) . | Sex . | Initial procedure . | Access way . | Technique of PH correction . | Mesh . | Outcomes . |
|---|---|---|---|---|---|---|---|
| Figiel and Figiel, 1967 | 76 | F | Loop colostomy | Laparotomy | Primary repair | No | Deceased |
| McAllister and D’Altorio, 1991 | 91 | F | End colostomy | Laparotomy | Stoma transposition | No | Discharge |
| Ellingson et al., 1993 | 77 | F | End colostomy | – | Primary repair | No | Discharge |
| Bota et al., 2012 | 41 | F | End ileostomy | Laparotomy | Primary repair | Yes | Mesh infection |
| Ilyas et al., 2012 | 93 | F | End colostomy | Laparotomy | Primary repair | No | Discharge |
| Ramia-Angel et al., 2012 | 64 | F | End colostomy | Refuse operative repair | None | No | Discharge |
| Marsh and Hoejgaard, 2013 | 81 | M | End colostomy | Laparotomy | Stoma transposition | No | Wound infection |
| Barber-Millet et al., 2014 | 69 | F | End colostomy | Laparotomy | Stoma transposition Preventive mesh of the new stoma | Yes | Discharge |
| Bull et al., 2017 | 85 | F | Loop colostomy | Laparoscopy convert to laparotomy | Stoma transposition | No | Discharge |
| Andrade et al., 2017 (current report) | 77 | F | End colostomy | Stoma site | Primary repair | Yes | Discharge |
The rarity of the gastric herniation into the herniary sac is explained in part by the numerous ligamentous attachments that keeps the stomach relatively fixed in the abdominal cavity. Ellingson et al. [3] believes that increased of gastric ligamentous laxity, like occurs in woman of advanced age with previous history of prior pregnancies, lets the stomach migrate from its native position to interior of the hernia.
Table 1 resume the main aspects of the nine cases previous described and the patient of this report.
In most published cases of gastric outlet obstruction as a consequence of PH, the most commonly used approach for correction of the complication was midline laparotomy (8/9 patients). In the present report, it was decided to access the contents of the herniary sac through an incision located in the place where the stoma had been made. The correction of the aponeurotic defect using a polypropylene mesh after approaching the edges of the herniary ring was also easily performed. The major advantage in correcting a PH by the site of the initial stoma compared to the technique of stoma transposition lies in the lower possibility of the development of incisional hernias at the site of the primitive stoma or in the midline incision used to access the cavity.
Several studies was done to evaluate the effectiveness and safety of open mesh repair comparing open non-mesh fascial repair with mesh techniques PH repair [10]. The study showed that mesh repair of a PH is safe and significantly reduces the rate of recurrence compared with primary sutured repair. Although these findings in the 10 cases of PH with gastric outlet obstruction presented in this report in only 3/10 cases the mesh was used. Regarding the way in which the mesh is placed to correct an PH by open access without the transposition of the stomach, the techniques that use the mesh cut like a keyhole are the most used. In the past, we used this technique, but the high rates of relapse would motivate us to cut the mesh like an ‘M’ letter as described in this article. With more than 50 cases of PH operated with this technique, we did not view extrusion of the mesh trough the stoma.
In summary, PH are a common late complication following stoma formation. In patients presenting with upper digestive obstructive symptoms, it is possible that this is due to gastric outlet obstruction secondary to stomach incarceration in the PH.
CONFLICT OF INTEREST STATEMENT
None declared.



