-
PDF
- Split View
-
Views
-
Cite
Cite
Shigeyuki Kanazawa, Koichiro Kiya, Tateki Kubo, Ko Hosokawa, Hydroxyapatite implantation for the repair of a congenital nasal anomaly: 10 years follow-up, Journal of Surgical Case Reports, Volume 2018, Issue 6, June 2018, rjy146, https://doi.org/10.1093/jscr/rjy146
Close - Share Icon Share
Abstract
Frontonasal dysplasia is a rare congenital anomaly characterized by ocular hypertelorism, a broad nasal root, and vertical median cleft of the nose and/or upper lip and palate. We report a case of frontonasal dysplasia in which hydroxyapatite was used to treat a nasal deformity in early childhood. In the 10 years of follow-up of our case, there were no complications such as infection, malpositioning, or exposure, and computed tomography revealed no resorption or malpositioning of the implant. Hydroxyapatite implants may be a viable alternative to autologous bone/cartilage grafts for the repair of congenital nasal anomalies until nasal development is completed.
INTRODUCTION
Frontonasal dysplasia is a rare congenital malformation characterized by hypertelorism, a broad nasal root, and vertical median cleft of the nose and/or upper lip and palate. In most cases, the nasal deformity must be repaired, with the addition of material to the nose for augmentation being preferred [1]. Structural nasal deformities are frequently addressed at the time of facial bipartition at 6–8 years of age, or shortly thereafter, using cantilever or L-strut bone grafts for nasal dorsal augmentation. Following this, revisionary rhinoplasty is usually needed to refine the nasal defects after nasal development is completed at age 14 or later [1]. Therefore, bone or cartilage grafts transplanted in early childhood must be removed and re-harvested at the time of revisionary rhinoplasty. In order to avoid wasting resources, hydroxyapatite can be used to treat the nasal deformity in early childhood as a substitute for autologous bone/cartilage grafts. Here, we present a mild case of frontonasal dysplasia and describe the surgical treatment for nasal deformity with 10 years of follow-up, in which hydroxyapatite was used to correct a nasal contour deformity.
CASE REPORT
An otherwise healthy 1-month-old infant was referred to our hospital for assessment of a nasal anomaly. Physical examination revealed a nasal deformity, including a broad nasal root, and absence of the nasal tip (Fig. 1). No nasal obstruction was found, and permeability of the bilateral nostril was within the normal range. There was mild ocular hypertelorism. Cranial structures were preserved, and there were no abnormal findings on neurological examination. A chromosomal test was normal, and there was no evidence of any other malformation. Other pediatric examination results were within the normal range.
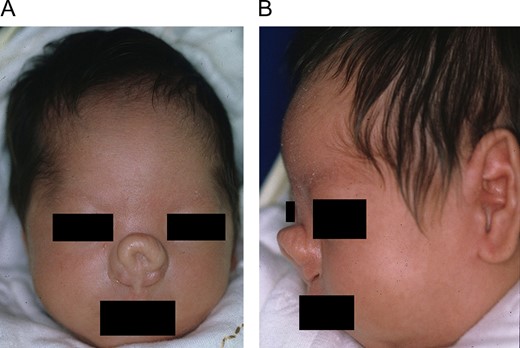
Physical examination revealed a nasal deformity, including a broad nasal root and absence of the nasal tip. (A) Frontal view. (B) Lateral view.
The patient has undergone four surgeries to date. She underwent her first open rhinoplasty to remove excess nasal skin at 11 months of age. During the operation, interdomal nylon sutures were used to approximate the medial crura because the bilateral alar cartilage was widely dilated.
The patient underwent a second operation for scar revision at 3 years of age and a third operation at 6 years of age for augmentation rhinoplasty (Fig. 2). For the third operation, hydroxyapatite implantation was performed for nasal contour augmentation. A transcolumellar incision was made at the level of the midcolumella, and subcutaneous tissue at the dorsum of the cartilage was dissected. A marginal incision connecting the columellar incision was made, and a flap was elevated. Dissection was carried out in a plane just above the perichondrium, a pocket was created, and a hydroxyapatite prosthesis was inserted (Fig. 3).
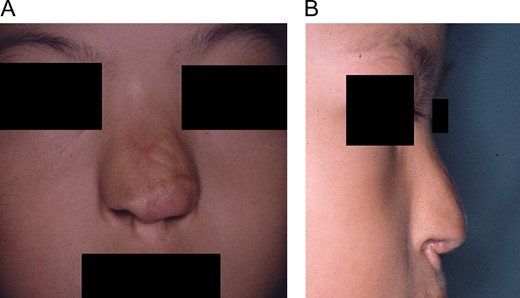
Frontal (A) and lateral (B) views before third operation at 6 years of age for augmentation rhinoplasty.

A hydroxyapatite prosthesis was inserted for augmentation rhinoplasty.
The patient was followed for 10 years after the third operation, and there were no complications, such as infection, malpositioning or exposure (Fig. 4). Computed tomography revealed no resorption or malpositioning of the implant (Fig. 5). A fourth operation (revisionary rhinoplasty) was performed to replace the hydroxyapatite prosthesis with an iliac bone graft at 16 years of age, after nasal development was completed.
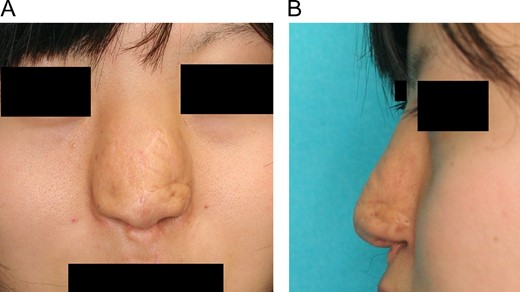
The patient was followed for 10 years after the third operation, and there were no complications, such as infection, malpositioning, or exposure of the hydroxyapatite implant. (A) Frontal view. (B) Lateral view.
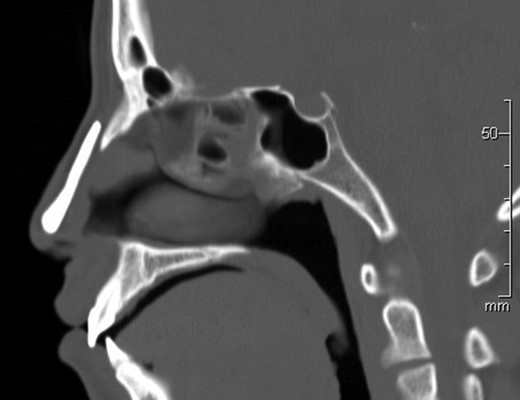
Computed tomography revealed no resorption or malpositioning of the implant 10 years after implantation.
DISCUSSION
Frontonasal dysplasia is a rare congenital anomaly of unknown etiology that can occur in isolation. Clinically, frontonasal dysplasia is defined as two or more of the following characteristics: (i) true ocular hypertelorism; (ii) broadening of the nasal root; (iii) median facial cleft affecting the nose and/or upper lip and palate; (iv) unilateral or bilateral clefting of the alae nasi; (v) lack of formation of the nasal tip; (vi) anterior cranium bifidum occultum; and (vii) V-shaped hair prolongation onto the forehead [2]. There are several classifications for frontonasal dysplasia. For instance, DeMyer [3] classified frontonasal dysplasia into four groups and three subtypes based on morphologic features. Sedano et al. [4] also proposed a classification based on embryological development, including four types with varying severity. The patient in our case had mild ocular hypertelorism, a broad nasal root and an absent nasal tip; however, cranium bifidum occultum frontalis was not observed. Based on these clinical features, our case was classified as DeMyer Type IV and Sedano Type A.
The nose plays an important role in facial esthetics, highlighting the need to reconstruct any congenital or traumatic nasal deformity. Although grafting for surgical reconstruction of nasal deformities is well reported, long-term outcomes are poorly documented, especially in children. A number of grafts and implants are available for use in nasal reconstruction and augmentation. Traditionally, autografts, such as from cartilage or bone, are the preferred choice because they have a high biocompatibility and low risk of infection, but disadvantages include the need for a donor site, which increases morbidity [5]. On the other hand, a variety of homografts and alloplastic materials are available, such as hydroxyapatite, silicon polymers, and polyethylene. Although these materials have some disadvantages with regard to biocompatibility and infection risk compared to autografts, they are advantageous in that they are free from donor-site morbidity. Considering the possibility that additional revisionary surgery will be needed to exchange the implant due to future facial growth, we believe it desirable to minimize donor-site morbidity, especially in childhood surgery. For this reason, we used hydroxyapatite as a substitute biomaterial for nasal reconstruction until nasal development is completed, after which it can be replaced with an autologous bone or cartilage graft in a revisionary rhinoplasty.
Hydroxyapatite is a component of bone and an implantable material. The use of hydroxyapatite for augmentation prevents donor-site morbidity, and the material is resistant to infection and biocompatible [5, 6]. Complication rates for such bone materials have ranged from 0 to 11%, and infection rates have been reported in up to 5% of cases [7–10]. In our case with 10 years of follow-up, there were no complications, and computed tomography revealed no resorption or malpositioning of the implant. Hydroxyapatite was successfully replaced with an autologous bone graft in a final revisionary rhinoplasty after nasal development was completed. In surgery for mild frontonasal dysplasia, hydroxyapatite can serve as an alternative to autologous bone or cartilage grafts to treat structural nasal deformities in early childhood until nasal development is completed at 14 years of age or later.
CONFLICT OF INTEREST STATEMENT
None declared.



