-
PDF
- Split View
-
Views
-
Cite
Cite
Hannah Buettner, Maria X Kiely, Mengdi Yao, James Yoo, Lilian Chen, Unique surgical approach to a twisted ileal-anal pouch, Journal of Surgical Case Reports, Volume 2018, Issue 6, June 2018, rjy133, https://doi.org/10.1093/jscr/rjy133
Close - Share Icon Share
Abstract
Total proctocolectomy with ileal pouch-anal anastomosis can restore gastrointestinal continuity in patients requiring colectomy for ulcerative colitis, however, it can be associated with high morbidity. Reoperation for pouch-related complications is technically challenging and often leads to deterioration of pouch function or need for permanent stoma. We report a case of acute on chronic small bowel obstruction secondary to a 360-degree twist in the small bowel introduced during creation of the ileal-anal pouch. Our novel approach at repair has not been reported in past literature which included resection and re-anastomosis of the small bowel proximal to the pouch allowing for pouch salvage with return to function.
INTRODUCTION
Total proctocolectomy with restorative ileal pouch anal anastomosis (IPAA) is commonly performed in patients with ulcerative colitis or familial adenomatous polyposis. In these patients, the procedure allows for restoration of gastrointestinal continuity but it can also be associated with high morbidity. We present an interesting case of a technical error that was created at the time of the initial pouch surgery which led to chronic obstructive pain. There are various ways of approaching this difficult clinical scenario and our surgical approach allowed for pouch salvage and return to function without increased morbidity to our patient. This unique technical approach has not been reported in past literature.
CASE REPORT
A 27-year-old male presented to our institution with 24 h of worsening acute on chronic abdominal pain and nausea. He had a history of ulcerative colitis for which he had a total proctocolectomy with mucosectomy and creation of IPAA 8 years prior to presentation. His past medical history was otherwise notable for primary sclerosing cholangitis which he had a liver transplantation with Roux-en-Y choledochojejunostomy 10 years ago.
Upon presentation, he was afebrile, normotensive, and not tachycardic. On exam, his abdomen was distended with minimal epigastric tenderness and no peritoneal signs. Laboratory evaluation was notable for a mild leukocytosis of 11.1 × 103 cells/μl. Abdominal CT scan with oral contrast showed dilated loops of small bowel with swirling of the mesentery directly proximal to the pouch with concerns for a volvulus (Fig. 1).
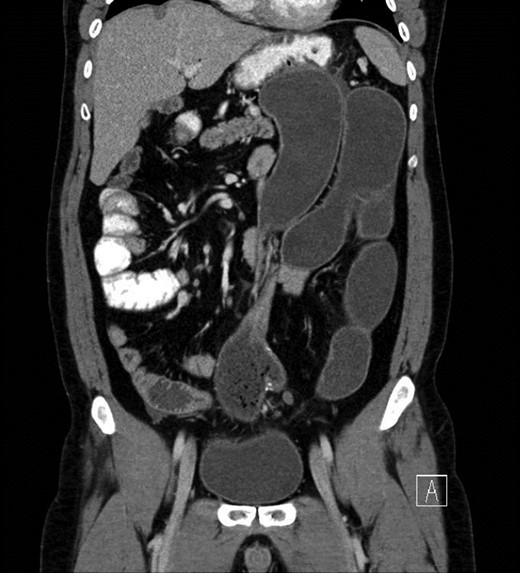
CT concerning for volvulus of small bowel proximal to pouch with proximal distended bowel.
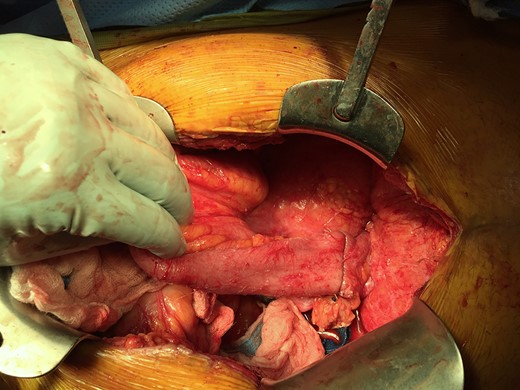
Decision was made to bring the patient to the operating room for exploratory laparotomy. Intra-operatively, he was found to have multiple distended loops of distal small bowel with wall thickening suggestive of a chronic process. The small bowel was evaluated from the ligament of Treitz; the small bowel anastomosis from prior choledochojejunostomy was identified and the Roux limb traced to the liver, then the distal limb was followed to the pouch, keeping the superior mesenteric artery straight. Immediately proximal to the pouch, a 360-degree twist in the short axis of the small bowel around the mesentery was identified (Fig. 2). Attempts at detorsion were unsuccessful. At this point, a pouchoscopy was performed, which revealed a straight, patent staple line without signs of intrinsic twist or volvulus of the pouch. Given the degree of small bowel dilatation, a diverting ileostomy was made proximal to the twist to allow for decompression and resolution of edema prior to attempting revision of the pouch. The patient recovered from this first surgery without complications. He also noted resolution of chronic pain he had associated with eating in the past.
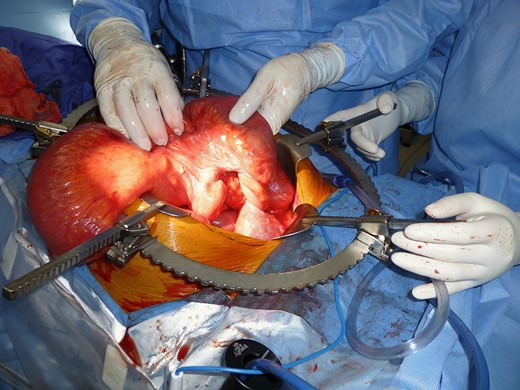
Intraoperative findings of ‘twist’ in the small bowel proximal to the pouch.
Prior to the patient’s pouch revision, we had multiple discussions regarding how to approach repair and salvage his pouch. One option would be to unseat the pouch and repeat the ileal-anal anastomosis. However, pouch revision in patients with prior mucosecectomy could be quite difficult and may result in injury to the pouch. An alternative option to preserve the pouch was discussed. This would consist of untwisting the bowel by resecting the twisted small bowel proximal to the pouch and performing an end to end anastomosis. The mesentery would not be transected and would remain twisted. Care must be given to preserve blood supply to the pouch or else loss of pouch could ensue.
The patient was brought back to the operating room eight weeks later, and the twist was repaired by resecting a small segment of small bowel and performing a primary re-anastomosis (Figs 3–5). This left a gentle twist in the mesentery; however, adequacy of blood flow to the pouch was confirmed by Doppler. Please see complete schematic illustrating our repair (Fig. 6). The patient returned to the operating room three months later for ileostomy reversal, and has had no recurrence of small bowel obstruction or issues related to pouch function in the following nine months.
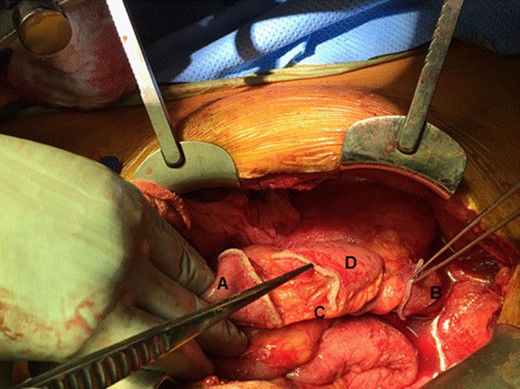
Novel repair option: small bowel proximal to the pouch was transected and subsequently resected. Figure shows disconnected small bowel proximally and distally. (A) proximal small bowel; (B) distal pouch; (C) mesentery feeding the pouch; and (D) portion of the small bowel to be resected.
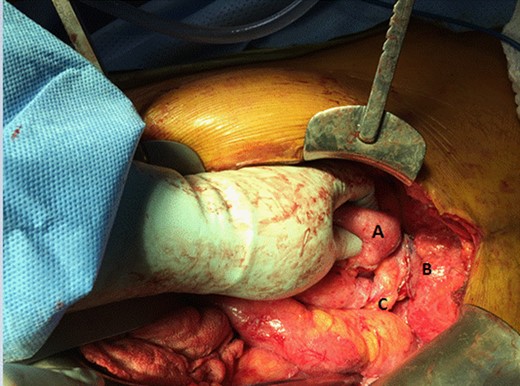
Small bowel has been resected. End to end anastomosis will be made from Point (A) to Point (B). Mesentery (C) is left ‘twisted’ behind the new anastomosis but blood supply to pouch maintained.
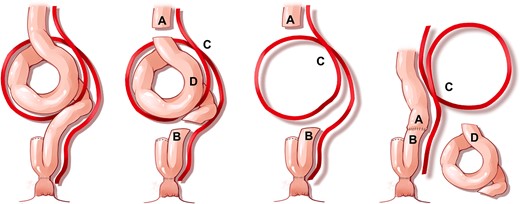
Schematic illustrating our repair: (A) proximal bowel, (B) distal pouch, (C) unresected, twisted blood supply/mesentery; and (D) resected small bowel.
DISCUSSION
Total proctocolectomy with IPAA is associated with a number of postoperative complications, the most common of which are small bowel obstruction (secondary to adhesions), pouchitis, strictures and fistulas [1]. Obstruction secondary to volvulus of the proximal small bowel or ileal pouch is rare, but a number of cases have been previously reported [2–6]. To our knowledge, this is the first report of a 360-degree short axis twist of the bowel introduced during the creation of the pouch repaired in this way. Revision of the pouch by unseating the pouch and repeating the ileal-anal anastomosis would correct the twist, but is not always feasible. This would require extensive pelvic dissection and potential injury to the pouch. Given the patient’s prior mucosectomy, there was also considerable concern regarding future pouch function. Our approach, resection and re-anastomosis of the small bowel with retained twist of the mesentery allowed for correction of the problem without need for revision of the prior anastomosis.
CONFLICT OF INTEREST STATEMENT
None declared.



